Longest-Lasting CAR T-Cell Therapy Success
A genetically engineered immune therapy known as CAR T-cell therapy has kept a patient free from a potentially fatal nerve tumor for an unprecedented 18 years. This marks the longest complete remission ever recorded in a patient treated with CAR T-cells.
“This is, to my knowledge, the longest-lasting complete remission in a patient who received CAR T-cell therapy,” says Karin Straathof from University College London, who was not involved in the treatment. “This patient is cured.”
How CAR T-Cell Therapy Works
Doctors use CAR T-cell therapy primarily to treat blood cancers such as leukemia. The process involves extracting a sample of T-cells from a patient’s blood, genetically modifying them to target and kill cancer cells, and then reinfusing them into the body.
In 2022, researchers reported that this approach had kept two leukemia patients in remission for about 11 years, which was the previous record. However, CAR T-cell therapy has struggled to combat solid tumors, such as neuroblastoma, due to their ability to resist immune system attacks.
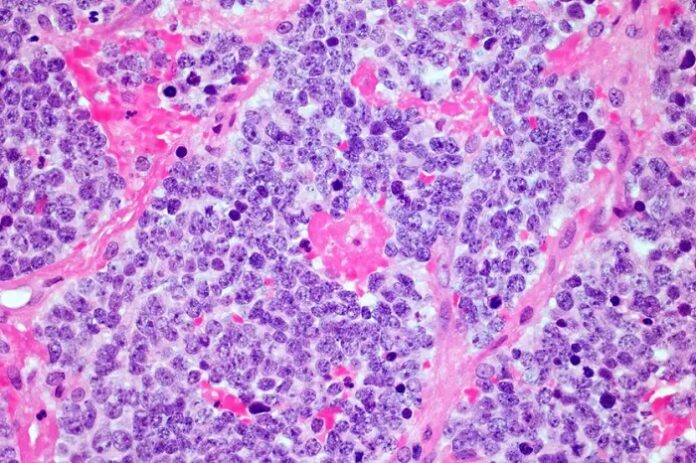
Breakthrough in Neuroblastoma Treatment
Cliona Rooney and her team at Baylor College of Medicine in Houston, Texas, were surprised to discover that a patient they treated with this therapy in 2005 remained cancer-free more than 18 years later. Neuroblastoma, a cancer that develops in nerve cells, typically affects children under the age of five and is particularly resistant to immune-based treatments.
“These results were amazing – achieving complete responses in neuroblastoma with this approach is quite rare,” says Rooney.
Trial Results and Patient Outcomes
As reported by newscientist, the patient received the therapy at age four after chemotherapy and radiotherapy failed to fully eliminate their cancer. At the time, the research team treated 10 other neuroblastoma patients whose cancer had relapsed following standard treatment. None experienced significant side effects.
One other participant remained cancer-free for nearly nine years before dropping out of the study, making further follow-up impossible. However, the remaining nine participants eventually died from their cancer, most within a few years of treatment.
Why Did Some Patients Respond Better?
Researchers remain uncertain about why certain patients responded significantly better than others. “That’s the $1 million question – we really don’t know why,” Rooney admits.
One possible explanation is that individual differences in T-cell behavior—shaped by genetics, prior infections, and lifestyle factors such as diet—played a role. The team also observed that CAR T-cells remained in the blood longer in patients who survived for extended periods.
Another factor could be the degree of immune suppression in some patients’ tumors, which may have made them more resistant to the CAR T-cell attack.
Advancing CAR T-Cell Therapy for More Patients
Rooney and her team are now working on improving this therapy to make it more effective for a broader range of patients. “We need to enhance these cells, making them more potent without increasing toxicities,” she says.
This groundbreaking case of long-term remission offers hope for the future of CAR T-cell therapy, paving the way for new advancements in cancer treatment.