*Dr. Reena J Wani, **Dr. Sachin S Paprikar
Abstract
The COVID-19 pandemic is the biggest threat in living memory to the human race. The Global havoc unleashed by the COVID-19 pandemic is unprecedented. As we complete more than 45 days since it was declared a pandemic, we review the available literature from across the world about everything related to COVID – 19 and women’s health, from conception to delivery. We present guidelines for antenatal care, testing, and precautions for health care workers [HCW]. Special emphasis is given on intrapartum care for COVID positive and suspected cases. We also present an algorithm for HCW exposed to possible cases.
Keywords: COVID-19 and pregnancy, Obstetric positive case, screening guidelines, PPE
Introduction
The COVID-19 pandemic is the biggest threat in living memory to the human race. In December 2019 a novel strain of coronavirus, officially named severe acute respiratory syndrome coronavirus 2 [SARS-Cov-2], was first isolated from three patients with coronavirus disease 2019 [COVID-19] by the Chinese Center for Disease Control and Prevention connected to the cluster of acute respiratory illness cases from Wuhan, China.
Since then the coronavirus pandemic has emerged to be the defining global health crisis of our time and the greatest challenge we have faced since World War Two. On 30th January 2020, the World Health Organization [WHO] declared that the outbreak of SARS-Cov-2 constituted a public health emergency of international concern, and on 11 March 2020 declared it to be a pandemic.
COVID-19, caused by severe acute respiratory syndrome coronavirus 2 [SARS-CoV-2], can cause acute respiratory distress syndrome [ARDS] and multiorgan failure, which is thought to result from a combination of virus-induced cytopathic effects and a dysregulated hyperinflammatory state, like in SARS. The incubation period is typically 5 to 7 days, with a range of 4-14 days. The diagnosis of current infection relies on tests to detect the presence of the virus in various body fluids. The standard test for diagnosis is the detection of viral RNA by molecular methods, typically a reverse transcription-polymerase chain reaction [RT-PCR] is recommended by the Indian Council of Medical Research [ICMR]. Antibody tests on blood are used to confirm past infection and presumed immunity to repeat infection, although the duration and effectiveness of such protection are not yet known. ‘Test, test, test’ is the key to controlling the spread and its clinical manifestation, according to the World Health Organization [WHO].
Current Scenario
|
COVID-19 CASES & DEATHS AS OF 4 MAY 2020 |
||
|
CASES |
DEATHS |
|
|
GLOBALLY |
3,356,205 |
238,730 |
|
INDIA |
29453 |
1373 |
|
SOURCE: GOVERNMENT OF INDIA COVID-19 Dashboard [https://www.mygov.in/covid-19] & WHO COVID-19 Dashboard [https://covid19.who.int/] |
||
COVID and Fertility: Should we be doing Assisted Reproductive Technology [ART]?
American Society for Reproductive Medicine [ASRM] recommends suspension of initiation of new treatment cycles, including ovulation induction, IUIs, IVF, and non-urgent gamete cryopreservation and continuation of care in cases that are urgent such as impending gonadotoxic therapy or extirpative reproductive surgery after necessary documentation supporting the same [1]. ASRM also recommends fertility experts to strongly consider cessation of embryo transfers, whether fresh or frozen, given the paucity of data surrounding the impact and potential risk of COVID-19 on pregnancy, the fetus, and child well-being [1].
As a precautionary measure the European Society of Human Reproduction and Embryology [ESHRE] has advised that – all fertility patients considering or planning treatment, even if they do not meet the diagnostic criteria for COVID-19 infection, should avoid becoming pregnant at this time. Preconception counseling in a hospital setting, for women with medical problems, should be deferred during the pandemic and replaced with advice to delay pregnancy and use reliable contraception [2].
COVID -19 and Pregnancy: Is the Prognosis Worse?
Currently, available data on COVID-19 does not indicate that pregnant women are at increased risk [3]. Though according to WHO, pregnant women do not appear to be at higher risk of severe disease; pregnant women are known to be at higher risk of severe morbidity and mortality from other respiratory infections such as influenza and SARS, making a strong case for pregnant women to be considered an at-risk population for COVID-19. Pregnant women with heart disease are at highest risk [congenital or acquired] [4].
Studies show pregnant women with COVID-19 infection showed a similar pattern of clinical characteristics to non-pregnant adult patients [5]. There are currently no data suggesting an increased risk of miscarriage or early pregnancy loss in relation to COVID-19 [6]. Adverse outcomes like preterm birth, premature rupture of membranes, fetal distress have been reported among mothers positive for COVID-19 during pregnancy[7]. However, this information is based on limited data and it is not clear whether these outcomes were related to maternal infection.
Though the limited case series of infants born to mothers infected with COVID-19 published in the peer-reviewed literature, none of the infants had tested positive for COVID-19[8], emerging evidence now suggests that vertical transmission is probable, although the proportion of pregnancies affected and the significance to the neonate IS yet to be determined[6]. Two reports have documented the presence of IgM for SARS-COV-2 in neonatal serum at birth, even though SARS-CoV-19 was not detected in the serum or throat swab by RT-PCR in any of these newborns [9][10]. A very small number of babies have tested positive for the virus shortly after birth, however, it is unknown if these babies got the virus before or after birth [11][12]. Currently there is no evidence to suggest that the development of COVID-19 pneumonia in the third trimester of pregnancy could lead to the occurrence of severe adverse outcomes in neonates [3]. The virus has not been detected in amniotic fluid, breast milk, or other maternal samples [3]. There is no evidence to say that SARS-COV-2 is teratogenic, long term data is awaited [2] [4].
Antenatal Care During the COVID-19 Pandemic: What Should be done? [2, 4, 6]
Women should be advised to attend routine antenatal care, tailored to minimum, at the discretion of the maternal care provider at 12, 20, 28 and 36 weeks of gestation, unless they meet current self-isolation criteria.
Individualized plans for women requiring frequent review may be necessary.
For women who have had symptoms, ANC appointments can be deferred until 7 days after the start of symptoms, unless symptoms become severe. Fetal Kick count to be maintained.
Symptomatic women should be evaluated as for non-pregnant cases and tested accordingly.
Testing for pregnant women should be done as per the latest ICMR testing strategy or state / local Govt guidelines. As per the current guidelines – pregnant women residing in clusters/containment area or in large migration gatherings/evacuees centre from hotspot districts presenting in labour or likely to deliver in the next 5 days should be tested even if asymptomatic.
If a woman meets the criteria for COVID-19 testing, she should be tested. Until test results are available, she should be treated as though she has confirmed COVID-19.
Obstetric management should not be delayed in order to test for COVID-19.
For women who are self-quarantined because someone in their household has possible symptoms of COVID-19, ANC appointments should be deferred for 14 days.
Any woman who has a routine appointment delayed for more than 3 weeks should be contacted.
Even if a woman has previously tested negative for COVID-19, if she presents with symptoms again, COVID-19 should be suspected.
Reducing routine growth scans where this is not for a strict guidance-based indication.
Referral to antenatal ultrasound services for fetal growth surveillance is recommended after 14 days following the resolution of acute illness.
Steroids should be given when indicated, there is no evidence to suggest that steroids for fetal lung maturation when they would usually be offered, cause any harm in the context of COVID-19.
COVID-19 Positive ANC Patient: What Next? [2, 4, 6]
It is mandatory for all hospitals [government and private], medical officers in government health institutions, and registered private medical practitioners including AYUSH Practitioners, to notify such patients with COVID-19 to concerned district surveillance unit.
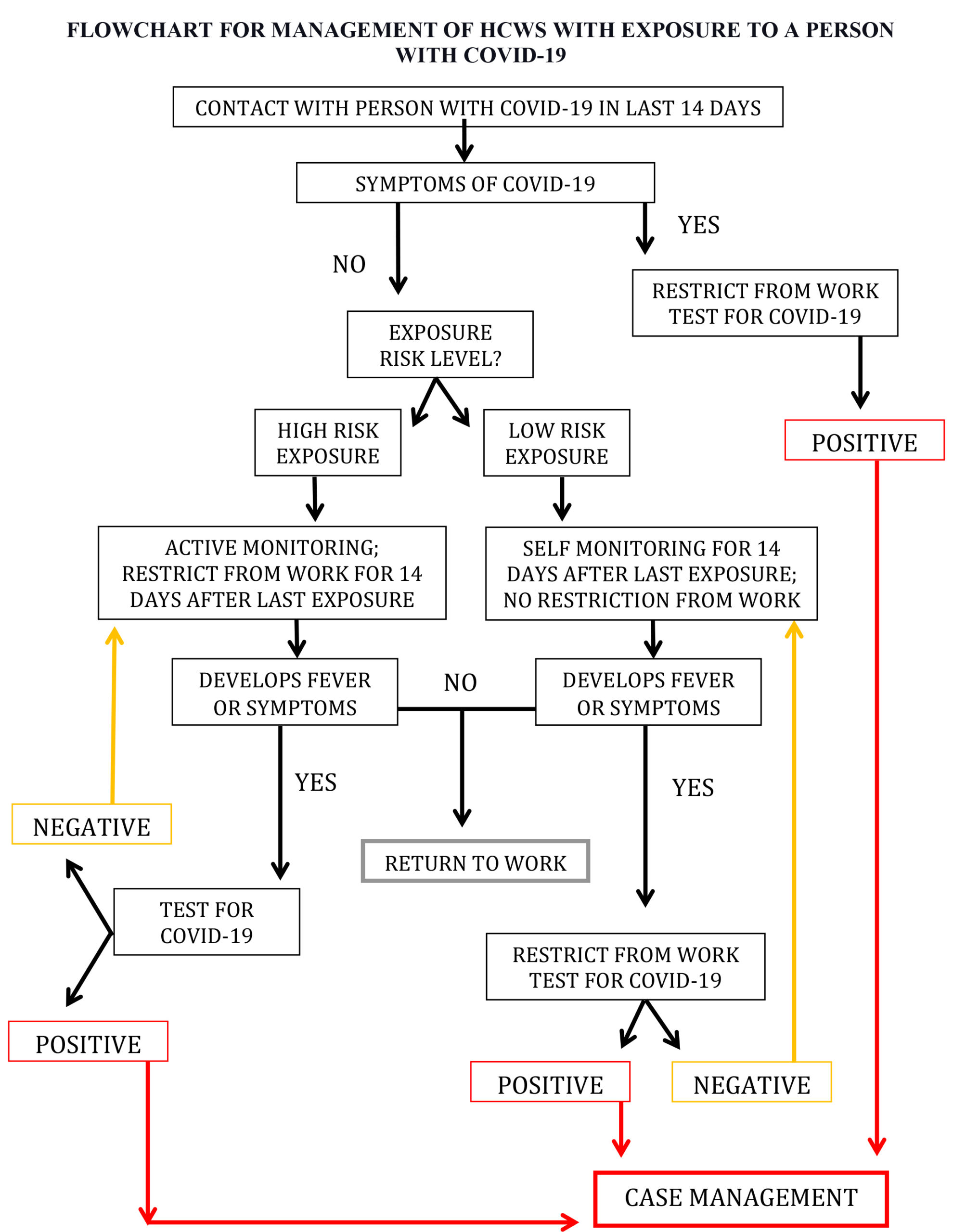
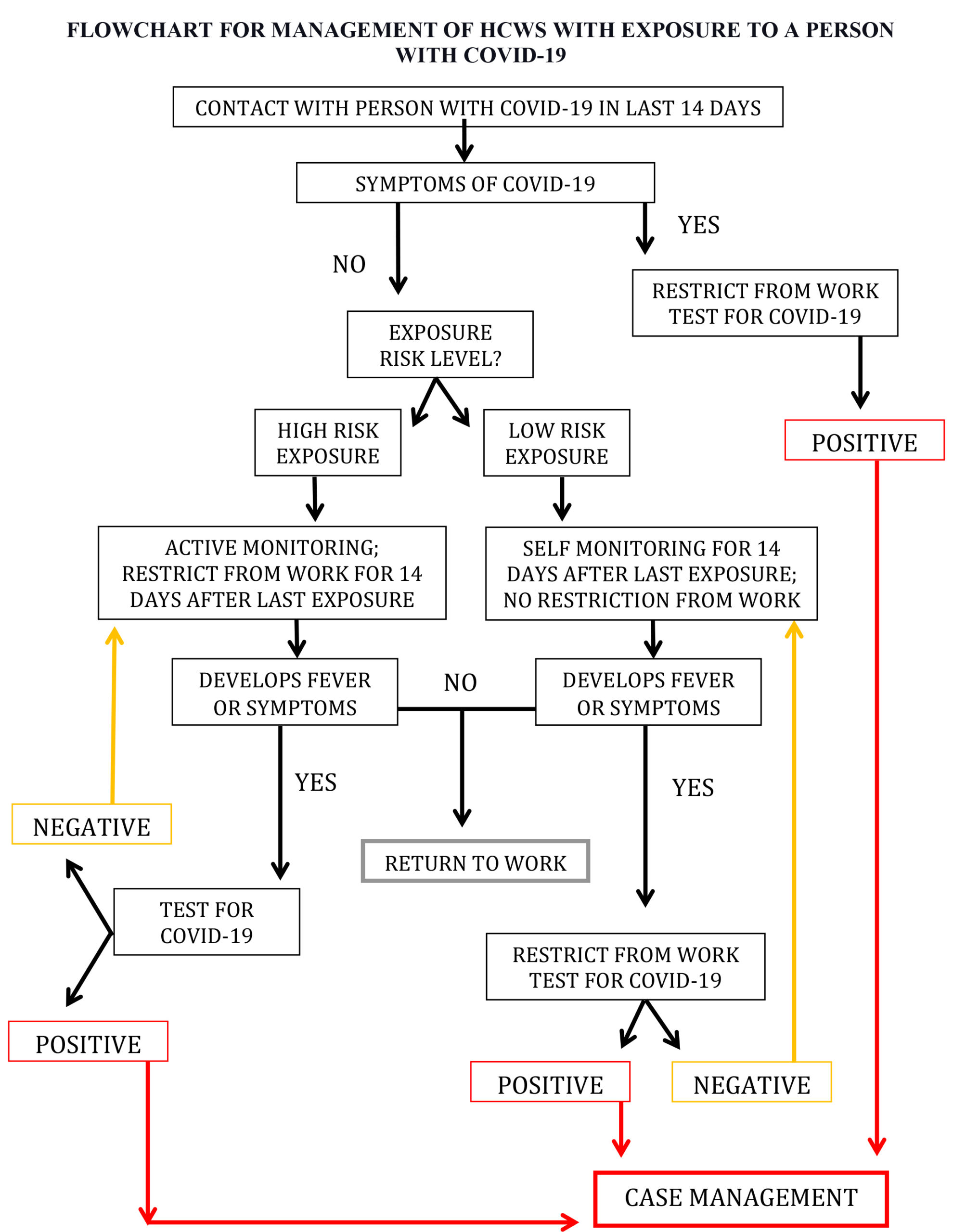
If a pregnant woman who has recently tested positive has attended ANC clinic in the last 14 days before testing, if so quarantine/ testing of the health care providers [HCP] based on the level of exposure and usage of personal protective equipment [PPE] [please check the flowchart for management of HCWs with exposure to a person with COVID-19 at the end of this article].
If a woman tests positive, she should be advised to deliver preferably at a designated COVID hospital or at least at an FRU [Rural/SDH] facility anticipating the complications during delivery.
ICMR guidelines dated 9th march, advice testing of all symptomatic health care workers. [13]
WHO recommends testing, stopping all health care interactions with patients for a period of 14 days after the last day of exposure to a confirmed COVID-his ar19 patient and quarantine for 14 days in a designated setting of HCWs exposed to COVID-19 virus at high risk for infection. [14]
Intrapartum Care for Pregnant Women with Suspected or Confirmed COVID-19 [2, 4, 6]
Once settled in an isolation room, a full maternal and fetal assessment should be conducted to include:
Assessment of the severity of COVID-19 symptoms, which should follow a multidisciplinary team approach including a medical specialist.
Maternal observations including temperature, respiratory rate & oxygen saturation.
Confirmation of the onset of labour, as per standard care.
Electronic fetal monitoring using a cardiotocograph [CTG].
Hourly oxygen saturation during labour.
There is an estimated incubation period for COVID-19 of 0-14 days [mean 5-6 days]; an infected woman may therefore initially present asymptomatically, developing symptoms later during an admission. HCPs should be aware of this possibility, particularly those who regularly measure patient vital signs.
If the woman has signs of sepsis, investigate and treat as per guidance on sepsis in pregnancy, but also consider active COVID-19 as a cause of sepsis and investigate according to guidance.
Care in Labour for Pregnant Women with Suspected or Confirmed COVID-19 [2, 4, 6]
Oxygen therapy should be titrated to maintain oxygen saturation >94%.
Continuous electronic fetal monitoring in labour is recommended.
Mode of birth should not be influenced by the presence of COVID-19 unless the woman’s respiratory condition demands urgent delivery. There is currently no evidence to favor one mode of birth over another. Hence the mode of birth and the timing should be individualized depending on the week of gestation and maternal, fetal, and delivery conditions.
Evidence says where vaginal secretions have been tested for COVID-19, the results have been negative.
For pregnant women with confirmed infection, in case of deterioration in the woman’s symptoms, an individual assessment regarding the risks and benefits of continuing the labour, versus emergency caesarean birth if this is likely to assist efforts to resuscitate the mother to be done.
An individualized decision should be made regarding shortening the length of the second stage of labour with elective instrumental birth in a symptomatic woman who is becoming exhausted or hypoxic.
There is no evidence that epidural or spinal analgesia or anesthesia is contraindicated even in the cases of confirmed infection. Epidural analgesia should, therefore, be recommended in labour to women with suspected/confirmed COVID19 to minimize the need for general anesthesia if urgent delivery is needed.
When caesarean birth or other operative procedure is being conducted, it should be done after wearing PPE.
Elective Caesarean Birth
In cases where elective caesarean birth cannot safely be delayed, the general advice for providing care to women admitted when affected by suspected/confirmed COVID-19 should be followed. [15]
Induction of Labour
Reducing induction of labour for indications that are not strictly necessary is recommended. [15]
An individual assessment should be made regarding the urgency of planned induction of labour for women currently in self-isolation because of suspected COVID-19 affecting either themselves or household contact. [15]
If induction of labour cannot safely be delayed, the general advice for services providing care to women admitted to the hospital when affected by suspected/confirmed COVID-19 should be followed. [15]
Pregnant Women with Moderate or Severe Signs – Symptoms of Suspected or Confirmed COVID-19 [2, 4, 6]
A multi-disciplinary team ideally involving a consultant physician, consultant obstetrician, and consultant anesthetist should be involved in managing the patient.
Hourly observations should include respiratory rate and oxygen saturation, looking for the number and trends.
The frequency and suitability of fetal heart rate monitoring should be considered on an individual basis, taking into consideration the gestational age of the fetus and the maternal condition.
Young fit women can compensate during deterioration in respiratory function and can maintain normal oxygen saturations before sudden clinical decompensation. Signs of decompensation include an increase in oxygen requirements or FiO2 > 40%, a respiratory rate of greater than 30, a reduction in urine output, or drowsiness, even if the saturations are normal. Escalate urgently if any signs of decompensation develop in a woman who is pregnant has recently given birth.
Oxygen should be titrated to keep saturation >94%.
Radiographic investigations should be performed as for the non-pregnant adult including chest X-ray and computerized tomography [CT] of the chest when indicated, and not delayed because of fetal concerns. Abdominal shielding can be used.
Additional investigations to rule out differential diagnoses e.g. ECG, CTPA, echocardiogram, and also full sepsis screening should be performed.
Bacterial infection should be considered if the WBC count is raised [lymphocytes usually normal or low with COVID-19] and antibiotics started.
Given the association of COVID-19 with acute respiratory distress syndrome [ARDS], women with moderate to severe symptoms of COVID-19 should be monitored using hourly fluid input-output charts.
Efforts should be targeted towards achieving neutral fluid balance in labour, to avoid the risk of fluid overload. Boluses in volumes of 250-500mls should be tried, assessment for fluid overload should be completed before proceeding with further fluid resuscitation.
RCOG recommends, all pregnant women admitted with COVID-19 infection [or suspected COVID-19 infection] should receive prophylactic low molecular weight heparin [LMWH], unless birth is expected within 12 hrs. The diagnosis of PE should be considered in women with chest pain, worsening hypoxia [particularly if there is a sudden increase in oxygen requirements] or in women whose breathlessness persists or worsens after expected recovery from COVID-19.
If urgent intervention for birth is indicated for fetal reasons, birth should be expedited as per routine obstetric practice, as long as the maternal condition is stable.
An individualized assessment of the woman, by the obstetrician along with the multi-disciplinary team, to decide whether emergency caesarean birth or induction of labour is indicated, either to assist efforts in maternal resuscitation or fetal or obstetric indications. It should consideration for the maternal condition, the fetal condition, the potential for improvement following elective birth, and the gestation of the pregnancy.
If maternal stabilization is required before intervention for birth, this is the priority, as it is in other maternity emergencies. The priority must always be the wellbeing of the woman.
COVID-19 and Breastfeeding
CDC documents, COVID-19 has not been detected in breast milk; however whether mothers with COVID-19 can spread the virus via breast milk is not known for sure.
In mothers with COVID-19 infection, informed decision to initiate breastfeeding should be taken by the healthcare provider after discussion with the mother and her family [16]. If the mother is sick and chooses to direct breastfeed, she should wear a facemask and wash her hands before each feeding. If the mother is sick and chooses to express breast milk, she has to wash her hands before touching any pump or bottle parts and before expressing breast milk. A dedicated breast pump should be provided. If possible, consideration should be given to have someone who is well, to feed the expressed breast milk to the infant [17].
Though the literature from China has advised separate isolation of the infected woman and her baby for 14 days, routine precautionary separation of a woman and a healthy baby should not be undertaken, given the potential detrimental effects on feeding and bonding. Given the current limited evidence, RCOG has advised that women and healthy babies, not otherwise requiring neonatal care, are kept together in the immediate postpartum period [6].
Discharge
Discharge for postpartum women should follow recommendations for discharge of hospitalized patients with COVID-19, two negative tests and maternal and fetal/neonatal conditions should be stable.
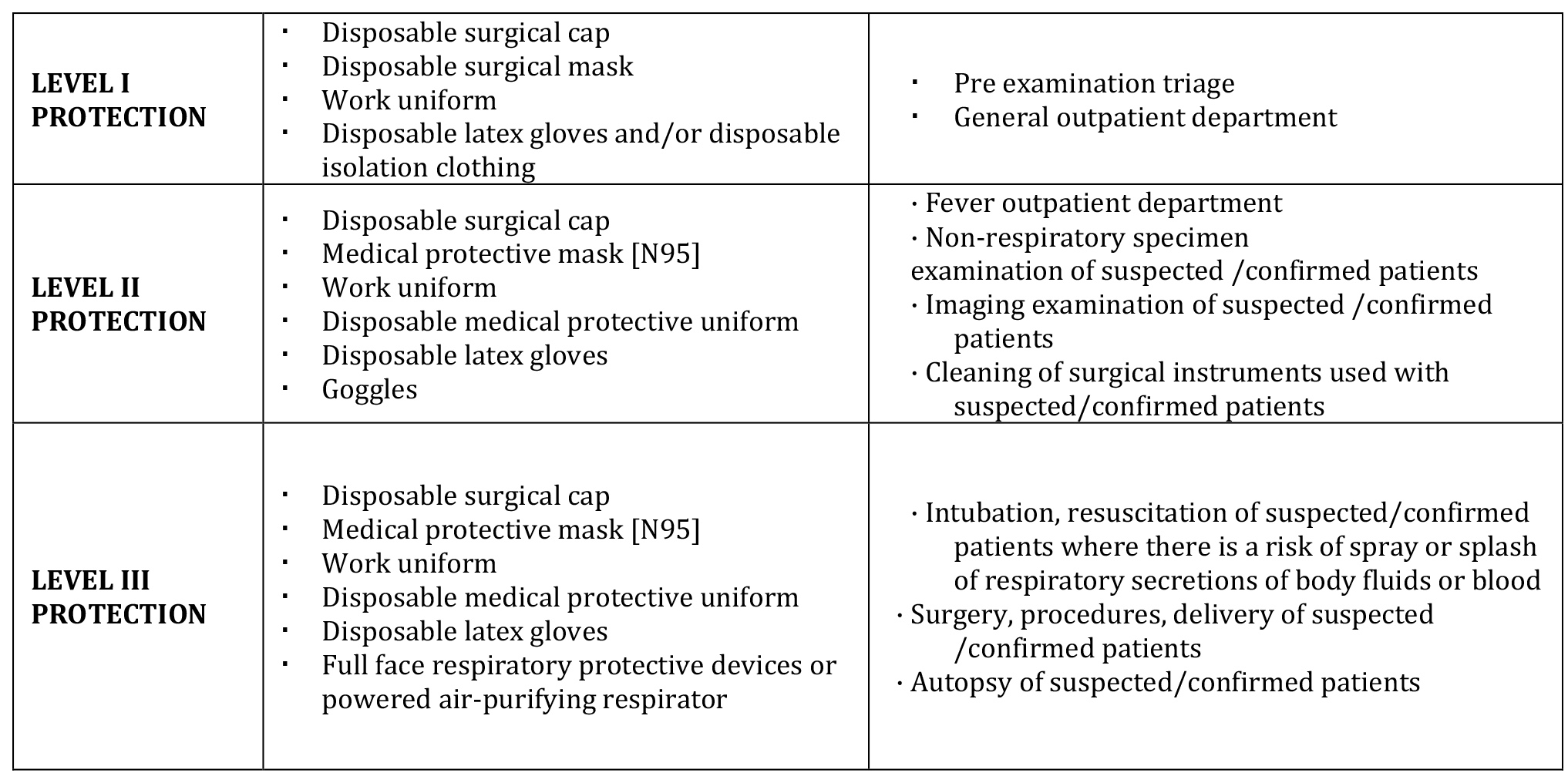
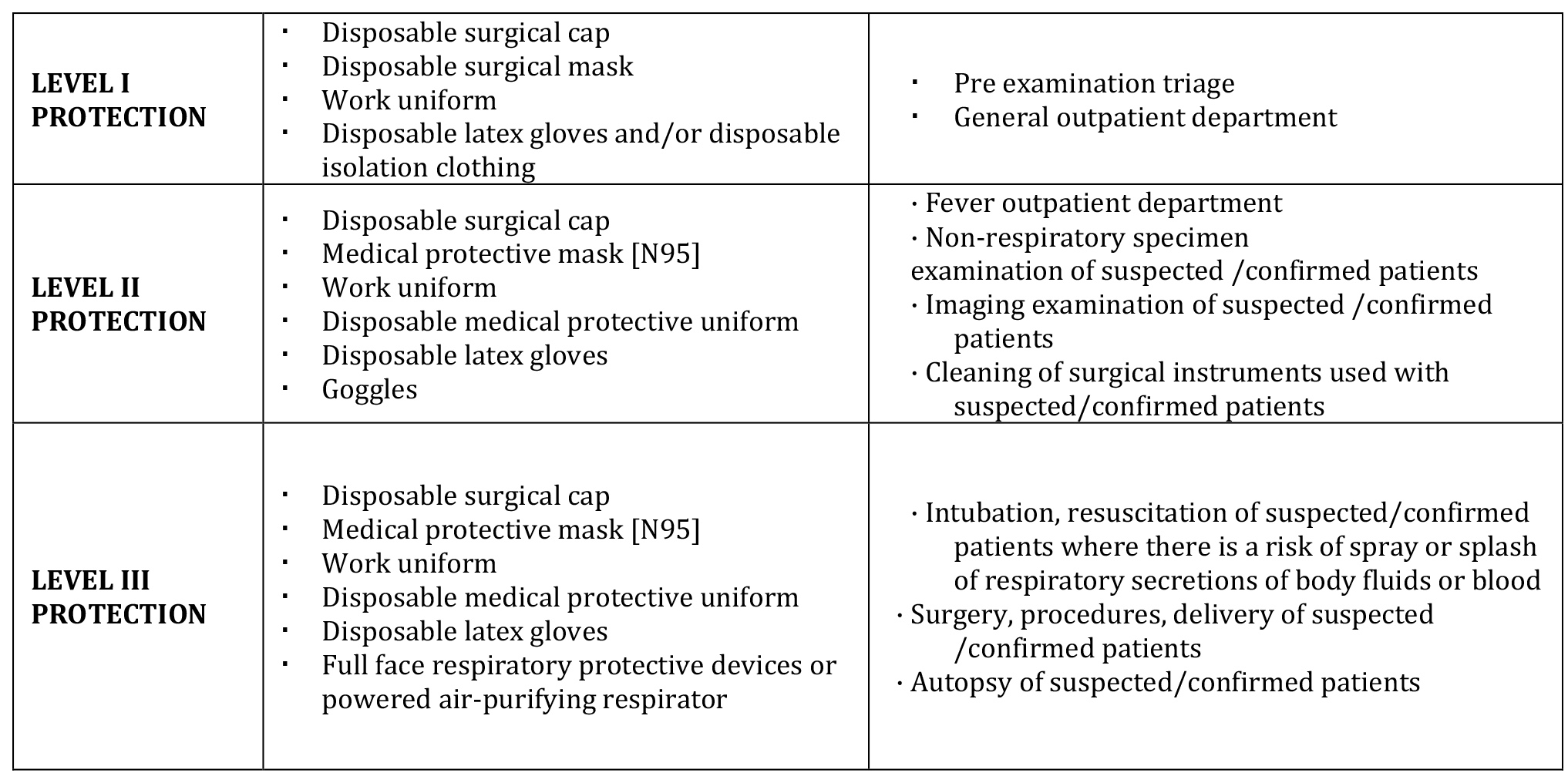
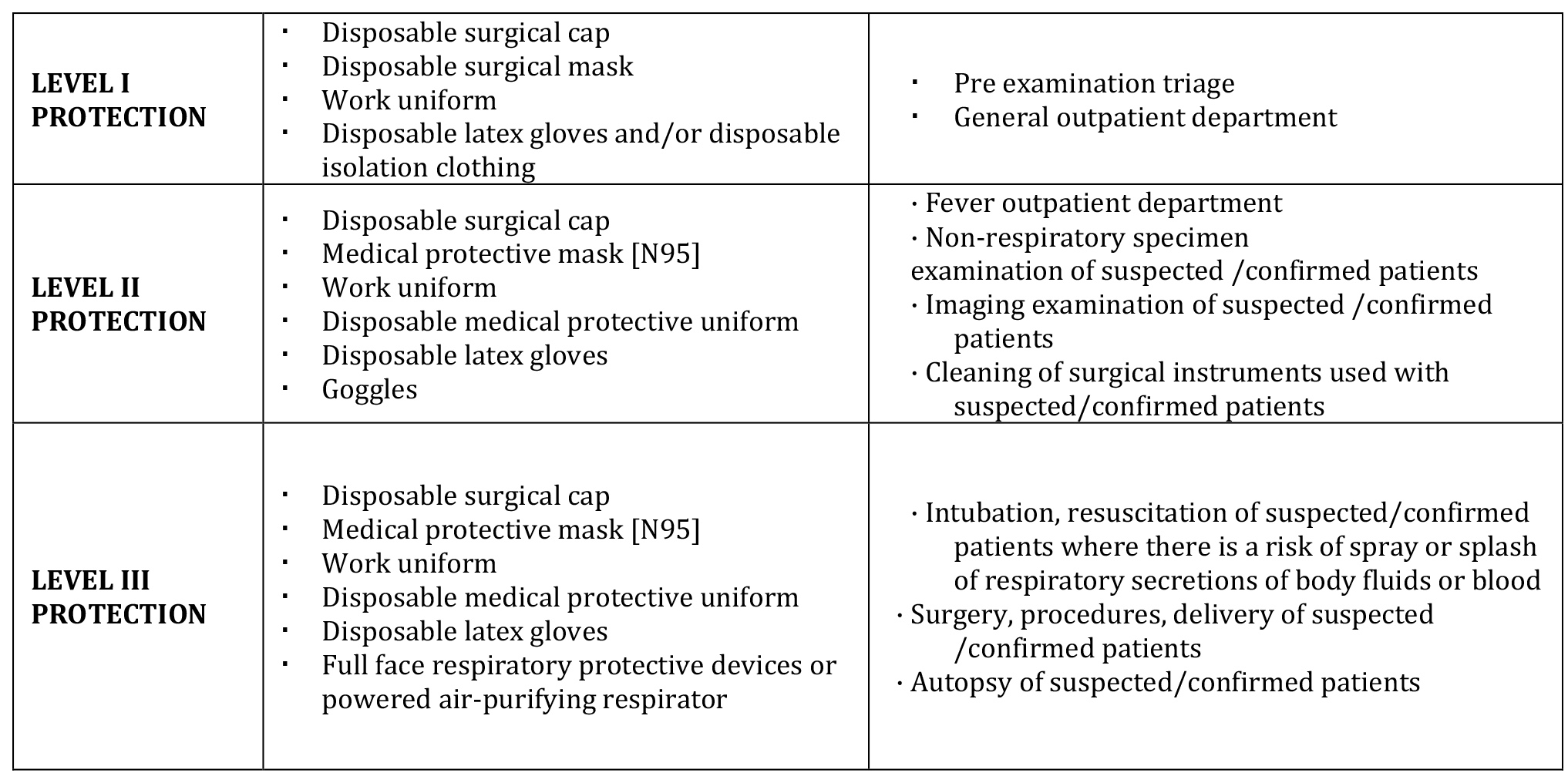
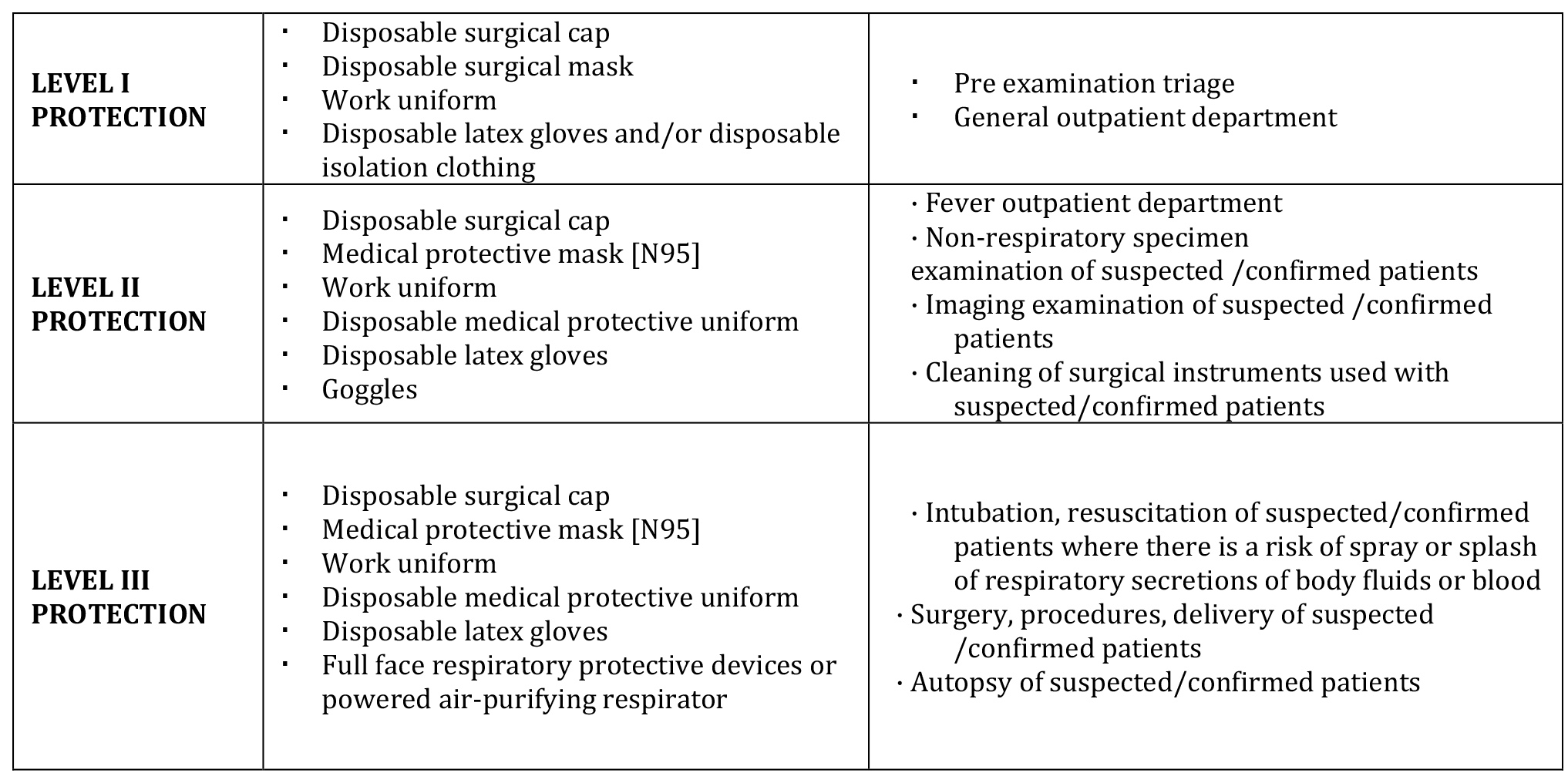
Personal Protection Equipment for Management of Suspected/Confirmed Case of COVID-19
Key Points for Clinical Practice During COVID-19 Pandemic
Planned pregnancy should be deferred.
Pregnancy outcomes are not significantly worsened by the COVID-19 pandemic.
Pregnancy itself is a state of relative immunosuppression and special care should be taken.
Asymptomatic pregnant women should be treated as per guidelines using telemedicine /staggered visits.
Symptomatic pregnant women need to be evaluated and treated aggressively.
ICMR guidelines require screening all pregnant women, even if asymptomatic from clusters/containment areas/ hotspots or in contact with COVID-19 cases.
Intrapartum hypoxia should be avoided, pulse oximetry, and pain relief to be provided.
LSCS for obstetric indications, preferably under regional anesthesia.
Breastfeeding may be permitted after counseling with due precautions.
While performing deliveries and procedures, the HCP should wear adequate PPE with full-body covering suit, N95 mask, and face shield.
FOOTNOTE:
High-Risk Exposure [18]
Close contact with a person with COVID-19 in the community; OR
Providing direct patient care for a patient with COVID-19 [e.g., physical exam, nursing care, performing aerosol-generating procedures, specimen collection, radiologic testing], without using proper personal protective equipment [PPE]2 or not performing appropriate hand hygiene after these interactions; OR
Having contact with the infectious secretions from a patient with COVID-19 or contaminated patient care environment, without using proper personal protective equipment [PPE] or not performing appropriate hand hygiene
Low-Risk Exposure – contact with a person with COVID-19 having not met the criteria for high-risk exposure.
NOTE: Where found necessary by the authors, the guidelines have been incorporated directly to ensure the exact meaning is conveyed.
References:
[1] ASRM. Patient Management and Clinical Recommendations During the Coronavirus[COVID-19] Pandemic. Available from: https://www.asrm.org/globalassets/asrm/asrm-content/news-and-publications/covid-19/covidtaskforce.pdf
[2] Coronavirus [COVID-19] infection and pregnancy [Internet]. Royal College of Obstetricians & Gynaecologists. [cited 2020Apr24]. Available from: https://www.rcog.org.uk/globalassets/documents/guidelines/2020-04-24-guidance-for-maternal-medicine.pdf
[3] Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, Li J, Zhao D, Xu D, Gong Q, Liao J, Yang H, Hou W, Zhang Y. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. The Lancet. 2020;395[10226]:809–15.
[4] Guidance for Management of Pregnant Women in COVID-19 Pandemic [Internet]. [cited 2020Apr24]. Available from:https://icmr.nic.in/sites/default/files/upload_documents/Guidance_for_Management_of_Pregnant_Women_in_COVID19_Pandemic_12042020.pdf
[5] Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, Li J, Zhao D, Xu D, Gong Q, Liao J, Yang H, Hou W, Zhang Y. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. The Lancet. 2020;395[10226]:809–15.
[6] Coronavirus [COVID-19] infection and pregnancy [Internet]. Royal College of Obstetricians & Gynaecologists. [cited 2020Apr24]. Available from: https://www.rcog.org.uk/en/guidelines-research-services/guidelines/coronavirus-pregnancy/
[8] Zhu H, Wang L, Fang C, Peng S, Zhang L, Chang G, Xia S, Zhou W. Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Translational Pediatrics. 2020;9[1]:51–60.
[9] Zeng H. Antibodies in Infants Born to Mothers With COVID-19 [Internet]. JAMA. 2020 [cited 2020Apr24]. Available from: https://jamanetwork.com/journals/jama/fullarticle/2763854
[10] Dong L. Possible Vertical Transmission of SARS-CoV-2 From an Infected Mother to Her Newborn [Internet]. JAMA. 2020 [cited 2020Apr24]. Available from: https://jamanetwork.com/journals/jama/fullarticle/2763853
[11] Zhang Z Wang C Gao CC. Neonatal coronavirus expert confirmed at 30 hours of birth: vertical transmission from mother to infant. Available from: http://www.cnr.cn/hubei/yuanchuang/20200205/t20200205_524961963.shtml
[12] Niu Y Yue H. Wuhan Tongji Hospital diagnoses first case of neonatal infection with new coronavirus. Available from: http://society.people.com.cn/n1/2020/0205/c1008-31572959.html
[13] INDIAN COUNCIL OF MEDICAL RESEARCH, DEPARTMENT OF HEALTH RESEARCH. Strategy for COVID19 testing in India [Version 4, dated 09/04/2020] Available from:https://icmr.nic.in/sites/default/files/upload_documents/Strategey_for_COVID19_Test_v4_09042020.pdf
[14] WHO Risk assessment and management of exposure of health care workers in the context of COVID-19: Interim guidance. Available from: https://apps.who.int/iris/bitstream/handle/10665/331496/WHO-2019-nCov-HCW_risk_assessment-2020.2-eng.pdf
[15] RCOG. Coronavirus [COVID-19] Infection in Pregnancy. Information for healthcare professionals Version 7: Published Thursday 9 April 2020. Available from: https://www.rcog.org.uk/globalassets/documents/guidelines/2020-04-17-coronavirus-covid-19-infection-in-pregnancy.pdf
[16] https://www.who.int/news-room/q-a-detail/q-a-on-covid-19-pregnancy-childbirth-and-breastfeeding
https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/pregnancy-breastfeeding.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fprepare%2Fpregnancy-breastfeeding.html
[17] https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/pregnancy-breastfeeding.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fprepare%2Fpregnancy-breastfeeding.html
[18] CDC. Coronavirus Disease 2019 [COVID-19]. Interim Operational Considerations for Public Health Management of Healthcare Workers Exposed to or Infected with COVID-19: non-US Healthcare Settings. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/non-us-settings/public-health-management-hcw-exposed.html#figure
*DR. REENA J WANI, Professor Addl & Head of Unit, Obstetrics & Gynecology
Correspondence: reena.wani@rediffmail.com
**DR. SACHIN S PAPRIKAR, S Registrar, Obstetrics & Gynecology
Correspondence: sachin.paprikar.nsk1@gmail.com
HBT MEDICAL COLLEGE & DR. R .N. COOPER HOSPITAL, MUMBAI.