Dr Tanu Singhal*
Abstract
COVID-19 has caused disruption, damage and death at an unprecedented scale. Knowledge about this disease is constantly evolving. The mode of transmission is believed to be primarily through droplet spread during face to face contact. In addition to the classical symptoms of fever, fatigue and breathlessness, loss of sense of smell and taste, skin manifestations and anorexia/ nausea/ diarrhea are emerging as new symptoms. The virus is now known to cause complications of almost all organ systems including blood vessels, heart, lung, kidney, brain and liver. The pediatric multi system inflammatory syndrome (PIMS) is a well-defined entity. Diagnosis is still by RT PCR in respiratory secretions. Obesity, genetic susceptibility have emerged as additional risk factors for severe disease. Evidence supports use of oxygen, anticoagulation, steroids and remdesivir in treatment of severe COVID-19. Steroids should not be given to non-hypoxic patients. Hydroxychloroquine, lopinavir ritonavir and azithromycin are no longer recommended for treatment. The jury is still out for tocilizumab and convalescent plasma. Patients can now be de-isolated 10-20 days after onset of symptoms for mild and severe disease respectively and demonstration of negative swabs is no longer essential. Vaccine development is underway.
Keywords: COVID-19, SARS-CoV-2, Remdesivir, Glucocorticoids, Tocilizumab, Convalescent plasma, Hydroxychloroquine
The COVID epidemic is now 7 months old causing a cumulative 20 million cases and 700,000 deaths worldwide. [1] India with 2 million cases and 40,000 deaths is the third worst affected country. [1] India is adding around 50,000 cases daily to the global case count. Our understanding about this virus has become better, yet there are more questions than answers; “The target is a moving one”. Here we shall discuss the latest updates on COVID-19 in a Frequently Asked Questions (FAQ) format. The answers to these FAQs are based on currently available evidence and guidelines and readers are urged to update themselves regularly.
What is the current consensus about transmission of COVID-19? [2]
COVID-19 is transmitted predominantly as a droplet infection generated during talking, coughing, sneezing during face to face contact. Face to face contact within 6 feet for more than 15 minutes, or staying in the same room for more than 2 hours increases transmission risk. The highest risk is for household contacts with secondary attack rates ranging between 30-50%. Transmission from inanimate surfaces contaminated with the virus is assumed to be less important than thought earlier. The role of transmission through small droplet nuclei suspended in air (airborne transmission) is still debated. Though the virus is excreted in stool, risk of faecal-oral transmission is uncertain.
Viral shedding starts 2-3 days before onset of symptoms and viral load peaks at the onset of symptoms. Transmission can occur from pre symptomatic/ symptomatic and asymptomatic individuals. It is believed that 48-62% of transmission of COVID-19 occurs from presymptomatic individuals as these people do not realize that they are sick and don’t follow infection control precautions. The basis of universal masking for all is primarily to cut down transmission from pre symptomatic/ asymptomatic individuals.
What is new about the clinical manifestations of COVID-19?
Apart from the earlier recognized symptoms of fever, myalgia, fatigue, cough and breathlessness, new symptoms are being described. Loss of sense of taste and smell has been described in up to 40% of the patients. [3] Skin manifestations are also being reported in between 5- 20% of patients. These include maculopapular rashes, urticaria, vesicles, petechiae, purpura, chilblains, livedo racemosa, and distal limb ischemia. [4] Recent studies have also described gastro intestinal manifestations including anorexia, nausea, diarrhoea, vomiting and abdominal pain in many patients either alone or associated with other manifestations. [5]
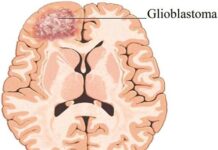
What new complications of COVID-19 are being recognized? [2, 6, 7]
The cytokine storm and attendant pneumonia and acute respiratory distress syndrome (ARDS) have been the commonest and the earliest recognized complications. However, what differentiates COVID-19 ARDS other causes of ARDS is widespread thrombosis in the pulmonary microvasculature, good toleration to hypoxia in initial stages (happy hypoxia/ silent hypoxia) and good lung compliance. COVID-19 has also emerged as a multi system disease since its target receptor ACE2 is found in multiple organs including the heart, endothelium, kidney, gastrointestinal tract, liver, endocrine system. [2] COVID-19 causes a prothrombotic state due to endothelial cell activation and consequent arterial and venous thromboembolism. Cardiovascular complications include myocarditis, heart failure, arrhythmias and myocardial infarction. Neurologic complications include strokes, encephalopathy and seizures. Adrenocortical insufficiency, hyperglycemia and ketosis are also being recognized and attributed to the virus attacking the endocrine cells. Acute kidney and liver dysfunction and hemophago lympho histiocytosis are other complications.
What is the optimal diagnostic algorithm for COVID-19? [8]
The gold standard test for diagnosis is RT PCR in respiratory secretions. These tests target two genes (one generic coronavirus) and one specific (SARS- COV-2). The turnaround time for these tests varies from 1-2 hours (Abbott point of care molecular test, Xpert Xpress and TruNAT) to 6-24 hours (Altona, Mylab, Thermofisher). The result is expressed as the cycle threshold; [Ct] high cycle threshold indicates a low viral load and vice versa. The cut off for defining a positive test varies with kits but is usually 40-45. Low Ct values correlate with early infection and high infectivity. The correlation of Ct values with disease severity is yet not established. The sensitivity of RT PCR depends on the site of collection; lower respiratory samples such as bronchoalveolar lavage and sputum have higher sensitivity (95% and 70% respectively) as compared to upper respiratory specimens including nasopharyngeal swab (50%), oropharyngeal swab (30%) and nasal swab (20%). Sensitivity is higher in early illness and also depends on the method of collection and transport.
Patients with suspected COVID (clinical symptoms, history of contact or epidemiology) and with a negative PCR test should be isolated and treated as probable COVID. The test may be repeated from a better site or a better kit. Here a CT scan may help since it often shows sub pleural ground glass opacities characteristic of COVID. [9] However, a negative CT scan does not rule out COVID, and similar appearances may be found in other viral infections. Hence while a CT should not be the first test for diagnosing COVID, it may be used in emergency situations for triaging sick patients presenting with breathlessness.
The antigen test for diagnosis of COVID-19 has recently become available in India. While it is point of care, highly specific and has a turnaround time of only 15 minutes, its sensitivity is only 20%. So while a positive antigen test unequivocally confirms COVID, a negative test does not rule it out and here a RT PCR is indicated. [10]
Antibodies appear 1-2 weeks after onset of infection and depend on severity of infection. Antibody tests that detect IgM and IgG or total antibodies are available as rapid tests (lateral flow assay), ELISA or CLIA. However these tests should not be used to diagnose acute infection. They are useful for retrospective diagnosis in patients who had previously tested negative by RT PCR or were not tested at all, for diagnosis of pediatric multi system inflammatory syndrome, for sero prevalence studies and for determining antibody content of convalescent plasma.
What are the predictors of serious COVID disease and mortality?
Current data indicates that 15-20% of patients with COVID-19 will need hospitalization of which 30% will need ICU care. [2] The overall case fatality rate is currently at 3%. [1] The case fatality rate depends on the degree of testing (widespread testing will lead to decrease in CFR), population demographics (countries with older population having higher CFR), access to health and critical care among other factors. The mortality rate in patients admitted to intensive care unit is around 30% and is 75-80% in patients who need mechanical ventilation. [11]
Host factors associated with worse outcomes include advanced age, being overweight/ obese, male gender, ethnicity, diabetes mellitus, hypertension, chronic pulmonary/ cardiovascular/ renal/ hepatic disease and immune-compromised state. [12] Apart from this, history of a close family member suffering from/ dying from COVID is also associated with adverse outcomes suggesting a genetic predisposition for severe COVID. [13]
Patients with persistent high fever beyond the first week, return of fever after an initial defervescence, breathlessness and exercise induced de saturation should be managed with caution since they indicate likelihood of a complicated course. Laboratory parameters indicative of severe disease include absolute lymphocyte count < 1000/ µl, neutrophil lymphocyte ratio off > 3.5, CRP higher than 60 mg/L, high D dimers (more than 6 times the cutoff), high ferritin and LDH (more than 600 µg/L and 600 Units/L respectively) and finally IL-6 levels more than 7-10 times of normal. [14,15] Extensive involvement on the CT scan also indicates worse outcomes.
How should mild COVID be treated? [16,17]
Mild COVID is defined as no clinical evidence of lower respiratory tract involvement, normal respiratory rate and oxygen saturation > 95% in room air. Patients with mild COVID can be treated at home provided i] facilities for isolation are available ii] there is reliable access to medical care iii] there are no major co-morbidities.
These patients should be treated with paracetamol on as need basis. Symptomatic therapy for nose block and cough may also be given. Vitamin C, Zinc and vitamin D are of unproven benefit but they may be prescribed for their placebo value. High doses of vitamin D should be avoided unless a low vitamin D level is documented. There are no food restrictions.
The use of hydroxychloroquine has not shown to be of any benefit in mild/ moderate COVID-19 in a recent randomized controlled trial and hence is not recommended at present. [18] There is no role of of azithromycin, ivermectin and doxycyline as well. Steroids must not be prescribed and may actually harm the patient by interfering with the host immune response. Favipiravir is an antiviral drug which acts by inhibiting RNA dependent RNA polymerase has been recently approved by the drug controller general of India in patients with mild/ moderate COVID-19. A couple of studies from China had shown faster viral clearance, shorter recovery time and better radiologic clearance with favipiravir as compared to lopinavir ritonavir/ umfenovir. [19, 20] Data from a RCT in 150 patients from India with mild/ moderate COVID-19 also showed faster resolution of symptoms with favipiravir as compared to standard of care. [21] The dose is 1800 mg twice daily on day 1 and then 800 mg twice daily for a total period of 14 days. However the ability of the drug to prevent progression to severe disease is unproven. Cases of progression to severe COVID despite early administration of favipiravir have been reported (personal communication, unpublished data).
Patients should be asked to monitor their temperature with a thermometer and oxygen saturation by a pulse oximeter after a 5 minute walk and report to emergency in case of breathlessness or drop in saturations. Laboratory investigations (CBC, CRP, LDH, D Dimer, etc) and CT imaging are not routinely needed. These may be done in patients worsening/ not improving after the first few days of illness
How should moderate COVID be treated? [16.17]
Moderate COVID is defined by the Ministry of Health and Family Welfare, India and the World Health Organization refers to patients who have a respiratory rate between 24-30 breaths per minute or those with oxygen saturation between 90-94%. In clinical practice, the management of these patients is almost similar to those with severe disease and will be dealt with in the subsequent section.
In real life setting, patients who have persistent fever beyond 5-7 days with/ without cough or CT evidence of pneumonia, but no hypoxia pose a significant treatment challenge. Data from the RECOVERY trial indicates that steroids should not be administered in the absence of hypoxia [22]. An interim analysis from the SIMPLE 2 study sponsored by Gilead suggests that use of remdesivir in non-hypoxic patients with CT finding of pneumonia was associated with reduced rates of disease progression [23]. Further data is awaited.
How should severe COVID-19 be treated? [2, 16, 18, 24]
Severe COVID is defined as patients who have a respiratory rate more than 30 breaths per minute or an oxygen saturation of less than 90% in room air. These patients should be admitted to the intensive care unit if possible
Baseline investigations include at least complete blood count, C reactive protein (CRP), creatinine, blood sugar, AST and ALT, urine routine, ECG and CXR. Other investigations depending on logistics/ availability include procalcitonin, CPK, LDH, D dimer, ferritin, Trop I, renal and liver function tests, CT chest with or without pulmonary angiography and screening 2D ECHO. Blood and other cultures should be sent if bacterial infections are suspected. Blood group and SARS- CoV-2 antibodies can be tested for if administration of convalescent plasma is planned.
Oral/ intravenous fluids should be given to maintain hydration. The patient should be started on supplemental oxygen with nasal prongs (for flow rates upto 5 l/ min) or face mask (flow rates of 6-10 l/ min) and face mask with non re breathing bag (for flow rates of 10-15 l/min) to maintain saturation at least > 90%. Awake proning has been proven to be beneficial in improving oxygenation and is strongly recommended. Patients with refractory hypoxemia should be put on high flow nasal oxygen (HFNO) if available and in preference to non-invasive ventilation with mask. [25] It is now believed that the benefits of non-invasive ventilation exceed the risk of virus aerosolization. However in patients with refractory hypoxemia, endotracheal intubation and mechanical ventilation is the only option. Adequate airborne transmission precautions should be taken during endotracheal intubation.
Low molecular weight heparin (LMWH) is indicated in all patients with severe disease to prevent thrombotic complications. Broad spectrum antibiotics should be given only if bacterial co infection is suspected. All patients should be started on corticosteroids as dexamethasone 6-12 mg/ day or methylprednisolone 30-60 mg/ day for 5-10 days. This recommendation of steroid use arises from the “RECOVERY” trial data that showed mortality benefit with use of dexamethasone 6 mg once daily for 10 days as well a historical control study from the Henry Ford Hospital System. [22, 26]
Remdesivir an antiviral drug which inhibits viral RNA dependent RNA polymerase has been shown in a recent randomized controlled trial to shorten the time to recovery from COVID-19 from 15 to 11 days and reduce mortality from 12% to 7% (albeit not statistically significant). [27] Further trials are in the offing. The drug is given as a loading dose of 200 mg intravenously followed by 100 mg daily for a total of 5 days; the US FDA recommends 10 days of therapy in mechanically ventilated patients. The dose in children is 5 mg/kg loading and then 2.5 mg/kg daily. The drug is contraindicated in pregnant and breast feeding women, those with creatinine clearance less than 30 ml/ minute and in those with liver enzymes more than 5 times of normal. At this time, the drug should be offered to all hypoxic patients with COVID-19 as early as possible since the RCT demonstrated that the drug was beneficial in the subgroup of patients on supplemental oxygen but not in those on mechanical ventilation.
Tocilizumab which is a monoclonal antibody against the IL-6 receptor has been used in the management of severe COVID-19. Several observational studies have demonstrated utility but interim data analysis from a recent randomized controlled trial did not show any benefit. [28, 29, 30] At present the drug is used in patients with severe hypoxia with high inflammatory markers (CRP and IL-6) where a bacterial infection has been ruled out. The dose is 4-8 mg/kg (maximum dose 800 mg) repeated if necessary after 12-24 hours. The main side effect is pre-disposition to severe infections both bacterial and fungal.
Convalescent plasma was purported to be beneficial in severe COVID-19 in observational studies. [31] However recent randomized controlled trials have not shown any impact on recovery and mortality rates. [32, 33] Till more information is available, convalescent plasma may be considered in patients with early disease who are baseline antibody negative.
Drugs which have not proven to be beneficial in severe COVID include lopinavir ritonavir, hydroxychloroquine with or without azithromycin. [34, 35] The role of other agents including anakinra, JAK2 inhibitors, sarilumab, itolizumab is being explored. [2]
The patients with severe COVID need very good critical care support. They need to be monitored for complications including arrhythmias, myocarditis, acute coronary syndrome, venous thrombo embolism and secondary bacterial and fungal infections. Extra corporeal membrane oxygenation (ECMO) has been practised in the resource rich settings. [24] There are anecdotal reports of successful lung transplant in patients with COVID-19.
What care should be offered post discharge?
Patients with severe lung involvement may need to go home on oxygen. Anticoagulants should be continued at discharge for patients who had documented thrombo embolism or those at high risk for VTE. [36] Patients should be asked to monitor oxygen saturation regularly. Readmissions in patients recovered from severe COVID are not uncommon; usual events are bacterial infections, intercurrent viral infections, evolving fibrosis, thromboembolic events and may be associated with morbidity and mortality. [37] Pulmonary function tests should be done on follow up and repeat CT imaging may be needed. Influenza and pneumococcal vaccination should be given if indicated.
How should patients who are asymptomatically infected with COVID-19 be managed? [38]
This is of common occurrence owing to testing of close contacts and testing prior to procedures and surgery. In the absence of symptoms it is difficult to ascertain whether the person is in the presymptomatic period, an asymptomatic carrier or in the post infectious phase. The Ct values may help to a certain extent; low Ct values indicating recent infection and high Ct values indicating late infection. [39] Irrespective of the Ct values, the patients should be isolated and monitored for development of COVID related symptoms for 10 days from the positive swab.
How should pregnant women with COVID-19 be managed? [40,41]
It is now a practice to test pregnant women routinely for COVID-19 in most cities in India. Many women are asymptomatic positive and these women have outcomes similar to their non-pregnant counterparts. However women symptomatic for COVID-19 with lower respiratory tract involvement tend to be at risk for maternal morbidity and preterm deliveries.
Intrauterine, intrapartum and breastfeeding related transmission is rare. Post natal transmission to neonates through close contact is also infrequent. Furthermore, most infected neonates are asymptomatic or have a mild illness. Therefore most authorities including the WHO and Indian Academy of Pediatrics recommend that unless the mother or the neonate need separation for managing their respective sickness, the babies should be roomed in with the mothers and breast feeding continued with the mother wearing a mask, practising good hand hygiene and keeping the baby’s cot at a distance of 2m from the mother’s bed. Routine vaccines including BCG, OPV and hepatitis B should be given before discharge.
How does COVID-19 affect children?
It is now well established that children are less often infected with COVID-19 and even if infected have mild disease. This may be due to better innate immunity, adaptive immunity due to exposure to other viruses, recent administration of vaccines including BCG and MMR, healthier lungs and immature ACE receptors. [42] Cases of severe COVID pneumonia and adverse outcomes are usually seen in infants and those with co morbidities.
However, a unique entity called paediatric multisystem inflammatory syndrome temporally associated with SARS-CoV-2 (PIMS-TS) is being recognized in children. [43] This syndrome is is due to an aberrant immune response to a previous COVID-19 infection. Children between the ages of 5-15 are most affected and present with high fever, rash, gastrointestinal symptoms including vomiting, abdominal pain and diarrhoea. They may also have conjunctival congestion, cracked lips. The manifestations mimic those of Kawasaki disease or bacterial toxic shock syndrome. These children may rapidly progress to shock and show reduced ejection fraction and coronary artery dilatation on echocardiography. The lungs are sparingly involved. Investigations show neutrophilia, normal or low platelet counts high CRP/ESR/ IL-6 levels/ ferritin and Trop I These children need very good critical care support and treatment with high dose steroids, intravenous immunoglobulin, aspirin, tocilizumab is indicated. With appropriate treatment, short term outcomes are good with rapid improvement in ejection fractions and coronary artery aneurysms.
While PIMS-TS is rare, doctors should keep a high index of suspicion in children presenting with fever and rash in the current day scenario. Differentiation from other tropical illnesses like dengue, rickettsial infections is also important.
What precautions need to be taken in health care facilities to prevent nosocomial transmission of COVID to other patients and health care workers?
This involves appropriate triaging of patients coming to hospital and admission of suspect and confirmed cases to isolation areas. Many hospitals and health care facilities in high transmission areas currently routinely screen for COVID-19 prior to/ at the time of admission and procedures. Health care workers in COVID areas should be in appropriate PPE with N 95 mask, eye protection, gown / body suits and gloves. Special care should be taken during aerosol generating procedures such as suctioning, intubation and tracheostomy. Even in non COVID areas, both staff and patients should be universally masked and practice proper hand hygiene. Patients and their relatives in non COVID areas should be monitored for development of COVID like symptoms and tested when necessary. All health care facilities should put in process protocols for monitoring, testing, isolating and treating HCW with COVID like symptoms.
Health care workers in OPD practice should use adequate PPE (surgical three ply mask with / without eye protection, gown and gloves) and practice good hand hygiene. They should use telemedicine whenever possible, space out appointments, limit entry of relatives and walk in patients, ensure masking by patients and relatives, keep face to face appointments short and ensure regular decontamination of OPD areas.
How long should patients with COVID-19 be isolated? [38]
There has been a paradigm shift in the recommendations for isolation. Earlier in the epidemic it was believed that patients shed virus for a prolonged period and isolation till two consecutive RTPCR’s were negative was advocated. This strategy was very resource intensive. However it was discovered over time that in most people viable virus was not isolated beyond day 9 of symptoms while the RT PCR continued to be positive for several weeks. [44] Hence it is now agreed upon that patients with mild disease or those who are asymptomatic positive can be de isolated 10 days from onset of symptoms/ positive swab and those with severe disease 20 days from onset of the illness if they have clinically recovered from the disease.
What is the degree of protection afforded by previous COVID against reactivation/ re infection?
This is probably “the” question in contemporary times. There is evidence of some degree of immunity against re infections i] as seen in previous studies on SARS-CoV-1 ii] studies in rhesus monkeys iii] very few re infections in the pandemic so far. [45] Though cases of recovered patients have been described who had positive RT PCR in throat with new symptoms, most of these patients did not have viable virus in the respiratory secretions and none of them transmitted infection to their contacts. [46] However the durability and longevity of infection associated immunity is not yet well established. It is also known that asymptomatically infected people/ those with mild infections have a weak immune response. This is the reason for reluctance to issue “immunity passports” to previously recovered patients. [47]
What are the currently recommended preventive strategies against COVID-19?
The main strategies continue to be social distancing, universal masking and hand hygiene. The role of BCG and MMR vaccines in boosting immunity and protecting from COVID-19 has not been established. Similarly post exposure prophylaxis with hydroxychloroquine was not found useful in a recent randomized controlled trial. [48] Pre-exposure prophylaxis with hydroxychloroquine while recommended for health care workers in India since the beginning of the epidemic has not been supported by robust trial data. [49]
There are many vaccine candidates in the offing. [50] Of these the frontrunners that have completed phase II trials and are undergoing phase 3 trials are Moderna pharmaceuticals mRNA -1273 vaccine, University of Oxford and Astra Zeneca’s AZD 1222 vaccine and Pfizer and BioNTech’s BNT 162 vaccine. Apart from these, vaccines from Russia, China are also going through phase 3 trials. In India, Bharat Biotech and Zydus Cadilla are evaluating indigenously developed vaccines in phase 2 trials while Serum Institute of India has tied up with AstraZeneca/Oxford and Novavax to mass produce vaccines. While the immunogenicity and safety data appears promising, the important question is whether the vaccines will be clinically efficacious.
What has been the impact of COVID-19 on society?
Apart from the direct effect on morbidity and mortality, the collateral effects of COVID-19 have been unprecedented. Attention to other illnesses especially cancer, transplant, HIV and tuberculosis has suffered. Life has changed across the globe; schools and businesses are closed. The psychological impact on the children, adults, elderly and health care workers has not even been measured properly. The economic impact runs in trillions of dollars and will be felt for decades.
What is the way forward?
Battling the epidemic requires efforts from all stakeholders including the government, society and health care sector. The responsibilities of health practitioners includes following infection control precautions to prevent acquisition of infection, keeping the self-updated about new developments, following the guidelines, recommending aggressive testing in patients with symptoms, using drugs rationally and referring patients to appropriate centres at the right time. At the same time it is the duty of the authorities and society to cooperate with health care workers and support them in all possible ways.
References:
- Johns Hopkins University of Medicine. Coronavirus research centre. Available at www. https://coronavirus.jhu.edu/. Accessed on August 8, 2020.
- Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 [COVID-19]: A Review. doi:10.1001/jama.2020.12839.
- Agyeman AA, Chin KL, Landersdorfer CB, Liew D, Ofori-Asenso R. Smell and Taste Dysfunction in Patients With COVID-19: A Systematic Review and Meta-analysis. Mayo Clin Proc. 2020;95[8]:1621-1631.
- Gottlieb M, Long B. Dermatologic manifestations and complications of COVID-19. Am J Emerg Med. 2020; 38[9]:1715-1721.
- Zarifian A, Zamiri Bidary M, Arekhi S, et al. Gastrointestinal and hepatic abnormalities in patients with confirmed COVID-19: A systematic review and meta-analysis. J Med Virol. 2020;10.1002/jmv.26314.
- Gavriatopoulou M, Korompoki E, Fotiou D, et al. Organ-specific manifestations of COVID-19 infection. Clin Exp Med. 2020;1-14. doi:10.1007/s10238-020-00648-x.
- Gupta A, Madhavan MV, Sehgal K, et al. Extrapulmonary manifestations of COVID-19. Nat Med. 2020; 26[7]:1017-1032.
- Sethuraman N, Jeremiah SS, Ryo A. Interpreting Diagnostic Tests for SARS-CoV-2. JAMA. 2020;10.1001/jama.2020.8259.
- Huang P, Liu T, Huang L, et al. Use of Chest CT in Combination with Negative RT-PCR Assay for the 2019 Novel Coronavirus but High Clinical Suspicion. Radiology. 2020; 200330.
- Indian Council of Medical Research. Newer Additional Strategies for COVID-19 Testing Dated: 23/06/2020. Available at https://www.icmr.gov.in/pdf/covid/strategy/New_additional_Advisory_23062020_3.pdf. Accessed on August 8,2020.
- Potere N, Valeriani E, Candeloro M, et al. Acute complications and mortality in hospitalized patients with coronavirus disease 2019: a systematic review and meta-analysis. Crit Care. 2020;24[1]:389.
- Xu L, Mao Y, Chen G. Risk factors for 2019 novel coronavirus disease [COVID-19] patients progressing to critical illness: a systematic review and meta-analysis. Aging [Albany NY]. 2020;12[12]:12410-12421.
- Yousefzadegan S, Rezaei N. Case Report: Death due to COVID-19 in Three Brothers. Am J Trop Med Hyg. 2020; 102[6]:1203-1204.
- Lippi G, Plebani M. Laboratory abnormalities in patients with COVID-2019 infection. Clin Chem Lab Med. 2020;/j/cclm.ahead-of-print/cclm-2020-0198/cclm-2020-0198.xml.
- Lee Dickens BS, Lim JT, Low JW, et al. Simple ‘Rule-of-6’ predicts severe COVID-19 disease. Clin Infect Dis. 2020; ciaa938. doi:10.1093/cid/ciaa938.
- Ministry of Health and Family Welfare, Govt of India. Clinical management protocol version 4. Dated 27/6/2020. Available at https://www.mohfw.gov.in/pdf/ClinicalManagementProtocolforCOVID19dated27062020.pdf. Accessed on August 8,2020.
- World Health Organization. Clinical Management of COVID 19. Dated 27/5/2020. Available at https://www.who.int/publications/i/item/clinical-management-of-covid-19. Accessed on August 2,2020.
- Cavalcanti AB, Zampieri FG, Rosa RG, et al. Hydroxychloroquine with or without Azithromycin in Mild-to-Moderate Covid-19. N Engl J Med. 2020;10.1056/NEJMoa2019014.
- Cai, M. Yang, D. Liu et al., Experimental Treatment with Favipiravir for COVID-19: An Open-Label Control Study, Engineering, https://doi.org/10.1016/j.eng.2020.03.007.
- Chen C, Zhang Y, Huang J et al. Favipiravir versus Arbidol for COVID-19: A Randomized Clinical Trial. Available at https://www.medrxiv.org/content/medrxiv/early/2020/04/15/2020.03.17.20037432.full.pdf. Accessed on August 8,2020.
- Glenmark announces top-line results from Phase 3 clinical trial of favipiravir for COVID-19 treatment. Available at https://www.expresspharma.in/covid19-updates/glenmark-announces-top-line-results-from-phase-3-clinical-trial-of-favipiravir-for-covid-19-treatment/. Accessed on August 4, 2020.
- RECOVERY Collaborative Group, Horby P, Lim WS, et al. Dexamethasone in Hospitalized Patients with Covid-19 – Preliminary Report. N Engl J Med. 2020;10.1056/NEJMoa2021436.
- Remdesivir shows clinical improvement in Phase III Covid-19 trial. Available at https://www.clinicaltrialsarena.com/news/gilead-remdesivir-phaseiii-trial-data/. Accessed on August 4,2020.
- Alhazzani W, Møller MH, Arabi YM, et al. Surviving Sepsis Campaign: Guidelines on the Management of Critically Ill Adults with Coronavirus Disease 2019 [COVID-19]. Crit Care Med. 2020;48[6]:e440-e469. .
- Raoof S, Nava S, Carpati C, Hill NS. “How I Do It: High Flow, Non-invasive ventilation and Awake [non-intubation] Proning in Covid-19 Patients with Respiratory Failure. Chest. 2020; S0012-3692[20]31910-3.
- Fadel R, Morrison AR, Vahia A, et al. Early Short Course Corticosteroids in Hospitalized Patients with COVID-19 . Clin Infect Dis. 2020; ciaa 601. doi:10.1093/cid/ciaa601.
- Beigel JH, Tomashek KM, Dodd LE, et al. Remdesivir for the Treatment of Covid-19 – Preliminary Report. N Engl J Med. 2020;10.1056/NEJMoa2007764.
- Somers EC, Eschenauer GA, Troost JP, et al. Tocilizumab for treatment of mechanically ventilated patients with COVID-19. Clin Infect Dis. 2020; ciaa954. doi:10.1093/cid/ciaa954.
- Patel K, Gooley TA, Bailey N, et al. Use of the IL-6R Antagonist Tocilizumab in Hospitalized COVID-19 Patients. J Intern Med. 2020;10.1111/joim.13163. doi:10.1111/joim.13163
- Roche’s Actemra fails to meet Phase III goals in Covid-19 patients. Available at https://www.clinicaltrialsarena.com/news/roche-actemra-covid-data/. Accessed on August 8,2020.
- Ye M, Fu D, Ren Y, et al. Treatment with convalescent plasma for COVID-19 patients in Wuhan, China. J Med Virol. 2020;10.1002/jmv.25882. doi:10.1002/jmv.25882.
- Li L, Zhang W, Hu Y, et al. Effect of Convalescent Plasma Therapy on Time to Clinical Improvement in Patients With Severe and Life-threatening COVID-19: A Randomized Clinical Trial JAMA. 2020; 324[5]:1-11.
- Gharbharan A, Jordans C, GeurtsvanKessel C et al. Convalescent Plasma for COVID-19. A randomized clinical trial. Available at https://www.medrxiv.org/content/10.1101/2020.07.01.20139857v1. Accessed on August 5,2020.
- Horby P, Mafham M, Linsell L. Effect of Hydroxychloroquine in Hospitalized Patients with COVID-19: Preliminary results from a multi-centre, randomized, controlled trial.Available at https://www.medrxiv.org/content/10.1101/2020.07.15.20151852v1. Accessed on August1, 2020.
- Cao B, Wang Y, Wen D, et al. A Trial of Lopinavir-Ritonavir in Adults Hospitalized with Severe Covid-19. N Engl J Med. 2020; 382[19]:1787-1799.
- American Society of Hematology. COVID-19 and VTE/anticoagulation: frequently asked questions. 2020. Available at:https://www.hematology.org/covid-19/covid-19-and-vte-anticoagulation.Accessed May 8, 2020.
- Rokadiya S, Gil E, Stubbs C, Bell D, Herbert R. COVID-19: Outcomes of patients with confirmed COVID-19 re-admitted to hospital. J Infect. 2020; 81[3]:e18-e19.
- Centers for Disease Control. Duration of Isolation and Precautions for Adults with COVID-19. Available at https://www.cdc.gov/coronavirus/2019-ncov/hcp/duration-isolation.html. Accessed on August3, 2020.
- Rao SN, Manissero D, Steele VR, Pareja J. A Narrative Systematic Review of the Clinical Utility of Cycle Threshold Values in the Context of COVID-. Infect Dis Ther. 2020; 1-14.
- Chawla D, Chirla D, Dalwai S, et al. Perinatal-Neonatal Management of COVID-19 Infection – Guidelines of the Federation of Obstetric and Gynecological Societies of India [FOGSI], National Neonatology Forum of India [NNF], and Indian Academy of Pediatrics [IAP]. Indian Pediatr. 2020; S097475591600154.
- Api O, Sen C, Debska M, et al. Clinical management of coronavirus disease 2019 [COVID-19] in pregnancy: recommendations of WAPM-World Association of Perinatal Medicine. J Perinat Med. 2020;/j/jpme.ahead-of-print/jpm-2020-0265/jpm-2020-0265.xml.
- Dhochak N, Singhal T, Kabra SK, Lodha R. Pathophysiology of COVID-19: Why Children Fare Better than Adults?. Indian J Pediatr. 2020; 87[7]:537-546.
- Whittaker E, Bamford A, Kenny J, et al. Clinical Characteristics of 58 Children With a Pediatric Inflammatory Multisystem Syndrome Temporally Associated With SARS-CoV-2. JAMA. 2020;e2010369.
- Wölfel R, Corman VM, Guggemos W, et al. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020; 581[7809]:465-469.
- Deng W, Bao L, Liu J, et al. Primary exposure to SARS-CoV-2 protects against reinfection in rhesus macaques . Science. 2020; eabc5343. doi:10.1126/science.abc5343
- Lu J, Peng J, Xiong Q, Liu Z, Lin H, Tan X, et al. Clinical, immunological and virological characterization of COVID-19 patients that test re-positive for SARS-CoV-2 by RT-PCR. [Preprint] Medrxiv. 2020. Available at: https://www.medrxiv.org/content/10.1101/2020.06.15.20131748v1
- Phelan AL. COVID-19 immunity passports and vaccination certificates: scientific, equitable, and legal challenges. Lancet. 2020; 395[10237]:1595‐1598.
- Boulware DR, Pullen MF, Bangdiwala AS, et al. A Randomized Trial of Hydroxychloroquine as Post exposure Prophylaxis for Covid-19.N Engl J Med. 2020; 383[6]:517-525.
- Indian Council of Medical Research. Revised advisory on the use of Hydroxychloroquine [HCQ] as prophylaxis for SARS-CoV-2 infection. Dated 22/5/2020. Available at https://www.icmr.gov.in/pdf/covid/techdoc/V5_Revised_advisory_on_the_use_of_HCQ_SARS_CoV2_infection.pdf. Accessed on August 1,2020.
- COVID-19 vaccine tracker. Available at https://www.raps.org/news-and-articles/news-articles/2020/3/covid-19-vaccine-tracker. Accessed on August8,2020.
*Consultant Pediatrics and Infectious Disease, Kokilaben Dhirubhai Ambani Hospital and Medical Research Institute, Mumbai.
Email: tanusinghal@yahoo.com