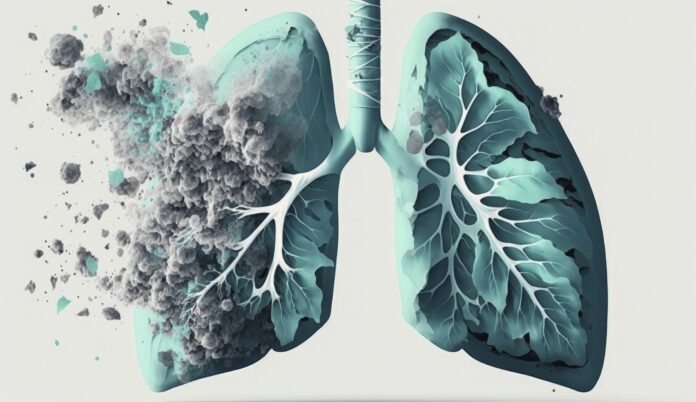
Non-smokers who develop non-small cell lung cancer (NSCLC) often exhibit a resistance to standard treatments, a phenomenon researchers believe is linked to genetic mutations. This insight was shared in a study published in Nature Communications.
Though smoking is a leading cause of lung cancer, the U.S. Centers for Disease Control and Prevention (CDC) states that 10% to 20% of lung cancer cases occur in non-smokers. The precise causes of lung cancer in non-smokers remain unclear, but experts suggest that genetic, environmental, and lifestyle factors may contribute.
Dr. Eric Singhi of the University of Texas MD Anderson Cancer Center noted that lung cancer among non-smokers ranks as the fifth leading cause of death globally, emphasizing that anyone with lungs is at risk. Although targeted treatments for NSCLC exist, their efficacy varies. Researchers from University College London, the Francis Crick Institute, and AstraZeneca have found that the presence of two specific genetic mutations might explain why these treatments fail in 10% to 15% of cases.
The study highlighted that mutations in the epidermal growth factor receptor (EGFR) gene, present in up to half of non-smokers with NSCLC, combined with mutations in the p53 gene, lead to drug-resistant tumors. Dr. Manmeet Singh Ahluwalia of the Baptist Health Miami Cancer Institute explained that these combined mutations result in tumors that often survive longer, with only a third of stage IV NSCLC patients with EGFR mutations living up to three years.
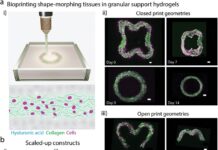
Typically, NSCLC is treated with EGFR inhibitors, but tumors with both EGFR and p53 mutations can grow despite treatment. Laboratory and animal studies demonstrated that these tumors, resistant to drugs, had more cancer cells with doubled genomes, making them prone to develop new drug-resistant cells.
Study co-author Charles Swanton, PhD, from the UCL Cancer Institute and Francis Crick Institute, stated that the combination of EGFR and p53 mutations, along with genome doubling, is linked to worse survival rates due to chromosomal instability.
Currently, NSCLC patients are tested for EGFR and p53 mutations, but there is no available test for genome doubling. Researchers are developing such a test, which could lead to more tailored treatments, such as early radiotherapy or combination therapies.
Dr. Shuresh Ramalingam of the Winship Cancer Institute of Emory University mentioned that when targeted treatments fail, molecular testing is performed to identify new mutations, guiding alternative interventions. He highlighted the emergence of experimental drugs to counter specific resistance mechanisms, such as the C797S mutation.
As reported by Medical News Today, the incidence of lung cancer among non-smokers has risen, particularly among women and younger individuals. Dr. Ahluwalia noted that two-thirds of these cases occur in women, making them twice as likely as men to develop lung cancer despite never smoking.