Summary
Hearing impairment is one of the important components of the universe of all the disabilities. Compromised hearing health varies in its type and severity. Increasing prevalence of hearing impairment, globally and in India, is due to an increase in the aging population related to improved longevity, environmental reasons like chronic exposure to rising noise pollution and to that of ototoxic substances. Impact of hearing impairment to any age group– children, adolescents and young or old persons has life-time adverse consequences influencing education, job opportunities, socialization and quality of life. While visual disability attracts sympathy from society, hearing impairment more often causes societal-ridicule. Community awareness, parental education, improved screening programs for hearing health at all levels of health care with established network for appropriate referral are the need of the hour. Hearing impairment is considered as a disability and the person/s affected can avail the assistance from the ADIP scheme of the Government of India provided he/she has a disability certificate that depends on the severity of the hearing impairment.
Introduction
Hearing loss (HL) is the most common sensory deficit in humans today. Hearing loss affects millions of people around the world and it is estimated to be the fourth leading cause of disability globally.[1] A person who is unable to hear the thresholds of 20dB in one or both the ears is said to have hearing loss. This hearing loss could range from mild, moderate to severe. Compared to normal hearing (-10 to 15dB), hearing loss can be classified as slight (16-25dB), mild (26 to 40dB), moderate (41-55dB), moderately severe (56-70dB), severe (71-90dB) and profound (>90dB).[2]
Studies from around the globe consistently show that rates of hearing loss have rapidly increased over the years. Within the decade 1985 to 1995, the numbers escalated from 42 million to 120 million.[3] The trends from Global Burden of Disease Study 2019, reviews the prevalence of hearing loss through a systematic study from 1990 to 2019, wherein the rates of affected population are 157 million.[4] Also, a 2021 assessment of WHO estimated 1.5 billion people living with impaired hearing.[4]
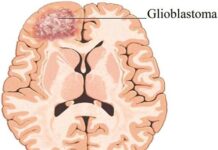
Hearing loss results due to congenital conditions, trauma, ear infections, diabetes, exposure to chemicals, exposure to loud noises, family history, tumours and medications. The connection between diabetes and hearing loss has been suspected for a long time.[5] It has been due to hyperglycaemic damage to the inner ear. It has been noted that, diabetics are more prone to hearing loss. This becomes very important in the Indian context with India being labelled as the diabetes capital of the world. In an Indian study conducted on 200 diabetic patients, 72% reported a mild sensorineural hearing loss and 20% had moderate sensorineural hearing loss.[6] In India, studies based on the prevalence of hearing loss are scarce. It is estimated that by the year 2050, one in every 10 people will have disabling hearing loss.[7] India has a double whammy of aging population and that of diabetes and as in India, being the diabetes capital of the world, the prevalence of HL population could be staggering. Hearing impairment impacts education and job opportunities, social relationships and comprehensively deteriorates quality of life. A call for public health concern has been voiced globally and in India.
Types and Causes of Hearing Impairment
Hearing impairment can occur in paediatric to geriatric groups; in new born, adolescent and young adults as well as in aged persons. Hearing loss can be categorised into three types: Conductive (involves outer or middle ear), Sensorineural (involves inner ear) and Mixed (combination of the two). The symptoms maybe mild, moderate, severe or profound. The cause for hearing loss can be hereditary and non-hereditary. Some of the causes are preventable or could be modulated by an early diagnosis and appropriate management viz. intrauterine infections, birth asphyxia, low-birth weight, hyperbilirubinemia, chronic ear infections, meningitis, smoking, otosclerosis, age-related degeneration, loud noise, and nutritional deficits. Rapidly rising loud noise from various sources like increase in noise pollution (occupation or entertainment industry). Hearing loss is commonly secondary to diabetes, aging, and tuberculosis. As hearing loss is caused by many factors, the important environmental and occupational causes are exposure to loud and prolonged noises, whereas, the underlying causes for hearing loss in paediatric and geriatric populations are commonly head trauma, inner and middle ear diseases and age-related hearing loss. Presbycusis, or age-related hearing loss, can be affected in one or both the ears which ultimately is resulted because of several health conditions like high blood pressure, diabetes, allergies and effects of medications.
Hearing Impairment and Consequences
The impact of unaddressed hearing loss can result and hamper various aspects like, communication and speech, cognition, education, employment, social isolation and stigma. This could have a negative impact on the society as well as the economy of one’s country. The psychological impact of hearing impairment may include everything from bullying, shame to aloofness. Trouble hearing can also affect one’s interpersonal communication skills at different social and personal events. As hearing loss, results in decline of several other important factors, the need of providing the appropriate assistance to balance the consequences is the necessity of an individual or it’s caregivers.
Assessment Tools for Hearing Impairment and Various Screening Programs
Screening can be addressed for different age groups such as new-born, school level, speciality clinics (diabetic and geriatric), at various stages. Prevention of hearing loss at an early stage and throughout the course of life is very important to reduce the number of individuals suspected of hearing loss. Effective strategies and implementation programs at various levels in association with local bodies needs to be carried in order to identify individuals with hearing loss at earlier stages. The World Report on Hearing (WRH) has been developed in response to the World Health Assembly resolution[4] (WHA70.13), adopted in 2017 as a means of providing guidance to integrate aural healthcare into National Health Plans. Hearing loss is one of the top five health conditions and diseases in which the number of years lived with a disability is significant.[8] Currently, babies born with risk factors are screened for hearing loss through behavioural and screening tools that include the use of noises makers and Otoacoustic Emissions (OAE) measurements, to go ahead with detailed Auditory Brainstem Response (ABR) testing if the babies fail the screening test. The Joint Committee on Infant Hearing recommends screening before hospital discharge, follow-up and diagnosis for infants needing additional care and the intervention and aural rehabilitation for infants identified with hearing loss. In adolescent and adults, Pure Tone Audiometry (PTA), a behavioural test can measure the individual’s hearing sensitivity. This testing is used to measure the air conduction and bone conduction responses of an individual through the earphones and vibrators respectively. Several Adult and Geriatric hearing loss questionnaires’ like HHIE, HEAR-QL, and HHL will help the audiologist to validate the results of their behavioural findings.
Services at Different Levels for Screening and Challenges
Hearing loss prevention at the primary level is the elimination of the onset and development of the problem. This is done by providing orientations and interactive programs to the target group, which includes medical and paramedical professionals guiding them regarding prevention, identification and management of HL through handbills, pamphlets and posters. Whereas, at the secondary level, it involves screening to identify individuals suspected to have HL. This is basically done by the audiologist and the ENT specialist by screening new-born babies at hospitals, school children, industrial workers and senior citizens as routine activity through noisemakers, hearing loss detection screening instruments, questionnaire and then subjectively based hearing test. Moreover, at the tertiary level, it involves rehabilitation of individuals identified with HL to be provided with intervention facilities in order to communicate effectively.
The challenges faced at the primary level include poor infrastructure as well as lower number of professionals to be a part of awareness programs, wherein, at the secondary level, funding and critical period of time in relation to fast recovery period are the major challenges of HL prevention.
In India, hearing disability is based on pure-tone hearing thresholds and speech discrimination score (PWD Act, 2001). As per PWD, individuals having hearing loss of less than 60 dB in the better ear will not be considered eligible as the total hearing disability will be less than 40%. In India, the minimum criteria to benefit from ADIP (Assistance to Disabled Persons for Purchase/Fitting of Aids and Appliances) scheme is having 40% of hearing disability.[9]
Diabetes and Hearing Loss
Tiwari and Mudhol reported a high prevalence (76.8%) of sensorineural hearing loss (SNHL) in patients with diabetes in India with a strong correlation between HbA1c, duration of diabetes and severity of SNHL.[10] Dosemane et al. have reported presence of bilateral hearing loss in 90.2% of diabetic patients.[11] Association of HL with type 1 and type 2 Diabetes Mellitus as well as with prediabetes is reported. However, prevalence of this association in Indian population has not been studied extensively.[12,13] Several studies have reported the association of uncontrolled glucose levels with hearing loss.[14]
The exact causal relationship between diabetes and hearing loss is not well established. However, many mechanisms are proposed for hearing impairment in diabetic patients including mitochondrial dysfunction, advance glycation end products, microangiopathy, inflammation, etc.
Hyperglycaemia is known to cause damage to mitochondrial DNA affecting the endocochlear function. Macroangiopathy because of uncontrolled diabetes leads to nerve damage in the inner ear. It is interesting to note that people with diabetes are at an increased risk for various kinds of complications and thus exposed to medications that can be ototoxic like certain anticancer drugs, aminoglycoside antibiotics, loop diuretics and so on.[14]
Hearing loss can significantly affect quality of life and may also affect a person’s earning capacity. Considering that there are 536.6 million people living with diabetes in the world today, all related complications like SNHL warrant screening.
Role of Nutrition
Besides well-known causes of HL like aging, exposure to loud noise and ototoxicity, nutrition also plays an important role in HL.[15] Findings from limited research on the role of macronutrients, tell us that carbohydrate intake may be associated with HL, through its effect on triglyceride levels. Isolated evidence is available for risk being higher for intake of foods with high glycemic index, higher glycemic load and if total CHO intakes are higher.[16] Besides higher carbohydrate, higher fat, cholesterol and low protein are also associated.[17] In a very recent study, Yévenes Briones et al. found that when 5% of the energy intake provided by saturated fatty acids was replaced by that from polyunsaturated fatty acids, the risk of disabling hearing function was 25% less among women but not men.[18] There is a possibility that n-3 fatty acids may be associated favourably with auditory function.[19,20] Whether consumption may be protective, although this needs to be verified, especially because animal studies do not provide this evidence.
Micronutrients play an important role either as antioxidants or because they have an essential role in the development and functioning of the ear. The importance of this is highlighted by improved auditory function with supplements. Vitamins that function as antioxidants could prevent the cochlear damage caused by reactive oxygen species both during and after exposure to noise. Anti-oxidant nutrients that have been studied include glutathione, N-Acetylcysteine, D-methionine, vitamin E, lipoic acid, coenzyme Q. Studies are also being done on these singly or in combination for use in rescue therapy. Vitamins and other micronutrients like magnesium are being studied as possible alternatives to chemical antioxidants.[15,21] In this context, it would be worthwhile to ensure that diets include those foods that are good sources of these nutrients as well as folate and vitamin B6. Folate and vitamin B12 are important because studies show that homocysteine is linked to hearing impairment; and FA supplementation has been shown to be capable of slowing the decline of auditory function at speech frequencies but not at higher frequencies. Iron and iodine deficiencies is of concern as it is linked to hearing loss in children.
Tinnitus has also been associated with single nutrients and dietary patterns. Higher intakes of calcium, iron and fat are associated with risk of tinnitus. Small controlled studies suggest that a diabetic diet rich in nutrients with a low-calorie, low-fat diet or healthy diets that characteristically contain more of fruits, vegetables and whole grains may confer a small benefit for diabetics with hyperinsulinemia.[22]
Ayurveda and How Hearing Impairment is Diagnosed
Hearing impairment has been described in Ayurvedic classics as karnabadhirya. Sushruta has described this as one of the 28 Karnarogas (diseases of ears) in great details.[23] Hearing loss has also been noted as one of the symptoms of Gut problems like Grahani and Krumi.[24] Among causative factors of hearing impairment stated in samhitasjara (old age) and Mithyayoga of shabda (exposure to abnormal sounds) are more, coinciding with current causes of HL. Genetic linkage has also been described in Sushruta.[25]
No description regarding Ayurvedic assessment of karnabadhirya is available.
Most of the causes vitiate Vata dosh and hence vatopkram (standard management of vatadushti) is recommended as the principle of management of Badhirya. Besides oral medicines such as Ghritapana, (intake of medicated ghee), Rasayanasevana, (Consumption of immunomodulators), Nasya (Instillation of medicated nasal drugs), and Karnapurana (Filling ear cavity with medicated oil) are recommended in management. Use of Bilvadi oil and Dashmool oil for local procedures like karnapooran[26] and karnabasti are in practice. Vaidya YG Joshi has treated 29 patients with HL by Bilvaditail[27] and found it to be beneficial within 2 months.[28-30] There are some reported clinical studies on use of Bilvaditailkarnapuran /basti and Karnabadhirya showing activity in HL, tinnitus and dizziness. Dr Dhananjay Kulkarni (ENT specialist) from Ahmednagar avails this Ayurvedic modality to treat his patients of HL and tinnitus. Sarivadivati and trikatukadiguti have been recommended in classics and are in practice.
Ayurvedic teaching institutes holds outpatient departments for karnaroga under Shalakya (Ayurvedic ENT) branch; however not much data on HL is available as compared to netra and nasaroga.
The Role of Audiologist and/or Speech Language Pathologist
Audiologists and/or Speech Language Pathologists play a major role in comprehensive care of individuals with hearing impairment. This collaborative effort is addressed for any age group and in any situation or setting.[31]
As per Indian Speech and Hearing Association (ISHA), Audiologist and Speech Language Pathologist (ASLP) have the scope of offering their expertise provided they have formal training and qualification specified by ASLP. The guiding principles for training and qualification have been largely derived from International Classification of Functioning Disability and Health (ICF) prescribed by the World Health Organization (WHO, 2001). The specialized expertise is not uniformly available at all levels of healthcare. However, its important role in multidisciplinary care is being gradually recognised and appreciated.[32]
Conclusion
The increasing number of people with hearing loss is a public health concern. However, the rising numbers of hearing loss-affected people can be brought under control by identifying the leading causes of hearing loss and implementing preventative actional programmes. Public health action is most needed to prevent hearing loss through control of various risk factors and ensuring that the needs of those who experience hearing loss can be provided with appropriate rehabilitation.
Acknowledgements
The authors wish to thank Dr Ashok B Vaidya, Prof Emeritus and former Research Director, Medical Research Centre, Kasturba Health Society for valuable inputs and constant support.
The authors also acknowledge Roda Dalal, Knowledge Cell-MRC-KHS for assistance in manuscript writing.
References
1. Cunningham LL, Lisa L. Hearing loss in adults. N Engl J Med. 2017;377(25):2465–2473.
2. Clark JG. Uses and abuses of hearing loss classification. ASHA. 1981;23:493-500.
3. Olusanya BO, Neumann KJ, Saunders JE. The global burden of disabling hearing impairment: a call to action. Bull World Health Organ. 2014;92(5):367-73.
4. Haile LM, Kamenov K, Briant PS, Orji AU, Steinmetz JD, et al. Hearing loss prevalence and years lived with disability, 1990-2019: Findings from the Global Burden of Disease Study 2019. The Lancet. 2021;397(10278):996-1009.
5. Samocha-Bonet D, Wu B, Ryugo DK. Diabetes mellitus and hearing loss: A review. Ageing Res Rev. 2021 Nov;71:101423. doi: 10.1016/j.arr.2021.101423. Epub 2021 Aug 9. PMID: 34384902.
6. Dayanand A, Dheebika J, Prathula S, Palaninathan S. A study on prevalence of hearing loss as a complication of diabetes. European Journal of Medical and Health Sciences. 2020:2(4). DOI https://doi.org/10.24018/ejmed.2020.2.4.405
7. Galhotra A, Sahu P. Challenges and solutions in implementing hearing screening program in India. Indian J Community Med. 2019;44(4):299-302.
8. The World Report on Hearing. Geneva: World Health Organization. 2021 https://apps.who.int/iris/bitstream/handle/10665/339906/9789240021501-eng.pdf
9. Shetty HN, Mathai JP, Uppunda AK. Disability certificate for individuals with hearing impairment – Time to rethink. Indian J Otol. 2017;23:7-12.
10. Tiwari A, Mudhol RS. Prevalence of sensorineural hearing loss among type-II diabetes mellitus patients attending KLES Dr. Prabhakar Kore Hospital and MRC: A cross-sectional study. Indian Journal of Health Sciences and Biomedical Research KLEU. 2018;11(2):165-169.
11. Dosemane D, Bahniwal RK, Manisha N, Khadilkar M N. Association between type 2 diabetes mellitus and hearing loss among patients in a coastal city of South India. Indian Journal of Otolaryngology and Head & Neck Surgery. 2019;71(2):1422-1425.
12. Baiduc R, Helzner E P. Epidemiology of diabetes and hearing loss. Seminars in hearing. 2019;40(4):281-291. https://doi.org/10.1055/s-0039-1697643
13. Cruickshanks K J, Dhar S, Dinces E, Fifer R C, Gonzalez F, Heiss G, et al. Hearing impairment prevalence and associated risk factors in the Hispanic Community Health Study/Study of Latinos. JAMA Otolaryngol Head Neck Surg. 2015;141(7):641-8.
14. Samocha-Bonet D, Wu B, Ryugo DK. Diabetes mellitus and hearing loss: A review. Ageing Res Rev. 2021;71:101423.
15. Puga AM, Pajares MA, Varela-Moreiras G, Partearroyo T. Interplay Between Nutrition and Hearing Loss: State of Art. Nutrients. 2018;11(1):35.
16. Gopinath B, Flood VM, McMahon CM, Burlutsky G, et al. Dietary glycemic load is a predictor of age-related hearing loss in older adults. J. Nutr. 2010;140:2207-2212.
17. Jung SY, Sang Hoon Kim SH, Yeo SG. Association of Nutritional Factors with Hearing Loss. Nutrients. 2019;11:307.
18. Yévenes‑Briones H, Caballero FF, Struijk EA, Lana A, Rodríguez‑Artalejo F, et al. Dietary fat intake and risk of disabling hearing impairment: a prospective population-based cohort study. Eur J Nutr. 2022;61(1):231-242.
19. Rosen S, Olin P, Rosen HV. Dietary prevention of hearing loss. Acta Otolaryngol. 1970;70:242–247.
20. Dullemeijer C, Verhoef P, Brouwer IA, Kok FJ, Brummer RJ, Durga J. Plasma very long-chain n-3 polyunsaturated fatty acids and age-related hearing loss in older adults. J Nutr Health Aging. 2010;14(5):347-51.
21. Pak JH, Kim Y, Yi J, Chung JW. Antioxidant therapy against oxidative damage of the inner ear: protection and preconditioning. Antioxidants (Basel). 2020;9(11):1076.
22. Dawes P, Cruickshanks KJ, Marsden A, Moore DR, Munro KJ. Relationship between diet, tinnitus, and hearing difficulties. Ear & Hearing. 2020;41;289-299.
23. KavirajaAmbikadatta Shastri Editor of Acharya Sushruta, “Sushruta Samhita” with hindi commentary “Ayurveda tattva sandipika” edited by-Chaukhambha Sanskrit Sansthan, Varanasi. 2011, Uttaratamtra, 21/38, page no.130.
24. Acharya Trivikrama Yadav and Narayanrao Acharya editer of Charak Samhita, Chokhamba Surbharati Prakashan Varanasi 2000, Grahani Chikitsa –cha chi 15/61, Pandu chikitsa -cha chi 16/13.
25. Kaviraja Ambikadatta Shastri Editor of Acharya Sushruta, “Sushruta Samhita” with Hindi commentary “Ayurveda tattva sandipika” edited by, Chaukhambha Sanskrit Sansthan, Varanasi,2011, Sutrasthan, 24/6.
26. Kaviraja Ambikadatta Shastri Editor of Acharya Sushruta, “Sushruta Samhita” with hindi commentary “Ayurveda tattva sandipika” Chaukhambha Sanskrit Sansthan, Varanasi. 2011, Uttaratamtra, 21/35,
27. Joshi YG. Book on Nivdak Rugna Chikitsa. Publisher; Pune Sahitya Vitaran.2009;51-54.
28. Sager AS, Khoja R, Vaghela DB. Management of Badhirya – Sensory Neural Hearing Loss with Ayurveda: A Case Report. International Ayurvedic Medical Journal. 2019; 7(5): 840-844.
29. Tyagi S, Bavalatti N, Rajagopala M. Management of Badhirya (hearing impairment) through Ayurvedic approaches: A case report. Journal of Ayurvedic Case Reports. 2021;4(1): 22-26.
30. Dash D K, Sharma A. A clinical study on Badhirya with Dashamulataila and Trikatukadigutiw.s.r to sensorineural hearing loss (SNHL). World Journal of Pharmaceutical Research. 2018;7(17):1014-1019.
31. Cherney LR, Gardner P, Logemann JA, Newman LA, O’Neil-Pirozzi T et al. Communication Sciences and Disorders Clinical Trails Research Group. The role of speech-language pathology and audiology in the optimal management of the service member returning from Iraq or Afghanistan with a blast-related head injury: position of the Communication Sciences and Disorders Clinical Trials Research Group. J Head Trauma Rehabil. 2010;25 (3):219-24.
32. Scope of Practice in Audiology and Speech-Language Pathology, November 2015, Rehabilitation Council of India, 3-12. Available from: https://www.ishaindia.org.in/pdf/Scope_of_Practice.pdf
+