Abstract
Hypertension is a highly prevalent modifiable cause of cardiovascular disease, stroke, and death. However, awareness, treatment, and control of high BP are very low, significantly increasing the risk of CVD and premature mortality and morbidity. Accuracy in BP measurement is critical, as even an error of 5-mmHg in measurement can lead to incorrect classification of hypertension in 84 million individuals worldwide. As the consequences of inaccurate BP measurement are grave, all the leading hypertension guidelines have placed a strong emphasis on accurate BP measurement. Achieving BP target goals is absolutely essential for significantly reducing composite cardiovascular outcomes in hypertensive patients.
Source of Support: None declared
Conflict of Interest: The author works with Aristo Pharmaceuticals Private Limited, Mumbai.
Introduction
World Hypertension Day is observed annually on May 17 to raise awareness of hypertension and encourage hypertension prevention, detection, and control. The World Hypertension League (WHL), an umbrella organization of 85 national hypertension societies and leagues, recognized that more than 50% of the hypertensive population worldwide are unaware of their condition. To address this problem, the WHL initiated a global awareness campaign on hypertension in 2005 and dedicated May 17 of each year as World Hypertension Day (WHD).In 2023, the theme is “Measure Your Blood Pressure Accurately, Control It, Live Longer”, focusing on combatting low awareness rates worldwide, especially in low- to middle-income areas, and accurate methods for blood pressure (BP) measurement.
High BP is a highly prevalent modifiable cause of cardiovascular disease (CVD), stroke, and premature death and it is one of WHO’s global targets for the prevention of non-communicable diseases.[1] According to WHO, approximately 1.13 billion people worldwide have hypertension,[2] and this figure has more than doubled since 1990.[1] Every year, hypertension is estimated to cause 9.4 million deaths worldwide.[3] It is estimated that 17.6% of hypertensive patients worldwide live in India, implying a significant increase in the burden of cardiovascular disease in the near future.[4] In India, the overall prevalence of hypertension is 30.7%, with men accounting for 34.2% and women accounting for 23%.[4] Recent epidemiological studies have reported that hypertension is present in 25-30% of urban and 10-20% of rural subjects in India; this translates into 100 – 110 million persons with this condition in the country.[5] There is a high prevalence of hypertension, with almost one in every three Indian adults affected.[4] Prevalence of hypertension in Indian young adults is also very high. Clinical studies have reported that among Indian young adults, 11.2% had hypertension and 33.3% had prehypertension.[6] Hypertension is currently a major public health issue in India, accounting for over 1.6 million annual deathsor 10.8% of total mortalities and 4.6% of disability-adjusted life years.[2]
Awareness, Control and Complications of High Blood Pressure
It is found that awareness, treatment and control of high BP among young adults with hypertension is very low.A community-based survey of the Indian population found that younger adults had less awareness of hypertension and its management than older people.[6] Approximately 25% of rural and 42% of urban Indians with hypertension are aware of their condition, and only 25% of rural and 38% of urban Indians are receiving treatment for their condition. Among them one-fifth of hypertensive urban Indians and one-tenth of those living in rural areas get their BP under control.[7] WHO estimates that just 12% of Indians with hypertension have their BP under control.[8]
Uncontrolled BP is one of the most important risk factors for CVD, which is the leading cause of mortality. Approximately 54% of strokes and 47% of coronary heart diseases, worldwide, are attributable to high BP[9] CVDs are also responsible for one-third of total deaths in India.[10]
The complications of high BP can be classified as short- and long-term consequences (Table1).[11]
Accurate BP Measurement – Essential Tool for Diagnosis and Management of Hypertension
Guidelines of Hypertension IV 2019
BP ≥130/80 is as per the ACC/AHA 2017 guidelines.
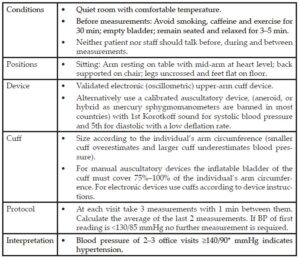
The accurate measurement of BP is essential for the diagnosis and management of hypertension. Accurate BP measurements ensure that patients receive correct health data and diagnoses, thereby assisting their overall physical wellness over the long term. Errors in the measurement of BP can lead to an incorrect diagnosis of hypertension. A 5mmHg error in BP measurement is estimated to result in the incorrect classification of hypertension status in at least 84 million people worldwide.[12] As a result, the consequences of inaccurate BP measurement on a global scale are grave.
Errors in BP measurement are a major source of BP misclassification and therefore the 2017 American College of Cardiology/American Heart Association and 2018 European Society of Cardiology/European Society of Hypertension clinical practice guidelines place strong emphasis on accurate measurement of BP by using validated devices and multiple readings for diagnosis and management of hypertension.[13]
Unfortunately, in modern clinical practice, BP measurement is frequently performed suboptimally, and this type of unstandardized BP measurement results in errors that can incorrectly alter management decisions in 20-45% of cases. Despite extensive education and significant efforts to raise awareness about the negative consequences of inaccurate clinic BP measurement, the problem of unstandardized BP measurement has persisted for decades.[12]
Ambulatory Blood Pressure Monitoring – Crucial Component of Hypertension Management
Historically, clinic or office blood pressure readings have been used for the diagnosis, treatment, and estimation of mortality risk in individuals with hypertension. According to the most recent research, the management of hypertension should include continuous ambulatory blood pressure monitoring as an integral part.
It is widely acknowledged that ABPM is a crucial component of good clinical practice in the field and plays a significant role in the diagnosis and management of hypertension.
The 24 – hour BP profile, comprising blood pressure variation, nocturnal hypertension, and morning BP surge, all of which are significant predictors of target organ damage and cardio- and cerebrovascular risk, can only be obtained using this approach, which is currently the only one available outside of an office setting.
Blood Pressure Reduction – Lower Premature Morbidity and Mortality
Randomized studies of blood pressure-lowering therapies have shown that pharmacological BP reduction is an effective method for lowering the risk of cardiovascular events in a variety of at-risk populations [15] Systolic BP reductions of 10 mmHg have been linked to a considerably lower risk of death, cardiovascular events, coronary heart disease, stroke, albuminuria, and retinopathy in hypertensive patients. Substantial proof that systolic and diastolic BP levels below 130 and 90 mmHg, respectively, are linked to less vascular complications has also been found in randomized clinical trials[5]. In a large-scale meta-analysis of randomized trials, a 5mmHg reduction in systolic BP lowered the risk of major cardiovascular events by 10%, irrespective of previous diagnoses of cardiovascular disease, and even at normal or high-normal BP values. These results imply that even at BP levels not typically recommended for treatment, a set degree of pharmacological BP lowering is equally effective for both primary and secondary prevention of serious cardiovascular disease.[15]
There has been a significant improvement in our understanding of the epidemiology, pathophysiology, and risk factors for hypertension, and a plethora of evidence show that reducing BP can significantly lower premature morbidity and mortality. This decrease in BP can be achieved using a variety of tried-and-true, highly efficient, and healthy lifestyle and pharmacological treatment. Despite this, globally as well as in India, BP control rates are still low and far from satisfactory.[16]
In India, less than one-fourth of hypertensive patients have their BP under control.[17] Thus, there is an urgent need for change and innovative solutions to lessen the burden of hypertension because both global and Indian efforts to control it have made slow headway. Better techniques are required to boost diagnosis and management, utilizing primary care or existing systems or developing novel concepts to involve consumers in BP management.[1]
Hypertension and Diabetes and Increased Risk of CVD
Hypertension and diabetes mellitus (DM) are two of the primary lifestyle disorders in the Indian and South Asian populations that commonly co-exist due to overlapping pathophysiology. Obesity, insulin resistance, inflammation, and oxidative stress are hypothesised to represent some common pathways. Diagnosis of type 2 diabetes mellitus has been made in up to 50% of hypertensive cases in India.[2] Individuals with diabetes demonstrated 1.5–2.0 times higher prevalence of hypertension than those without diabetes. Cardiovascular risks, end-organ damage, and renal problems are the key issues linked to diabetic hypertension that needs to be addressed with the use of non-pharmacological and pharmacological methods.[2]
BP Target Goals
SPRINT trial published on November 2015, showed that intensive BP control to SBP <120 mmHg results in significant cardiovascular benefit in high-risk patients with hypertension compared with routine BP control to <140 mmHg.[18]
Based on the results of the SPRINT trial many of the international guidelines on hypertension (2017 ACC/AHA guidelines, 2018 ESC/ESH, the 2019 Canadian Hypertension Education Program (CHEP) guidelines) further lowered the BP control goals.
Both the ACC/AHA and ESC/ESH recommends target BP of <130/80 mmHg for hypertensive patients with or without comorbidities like diabetes, chronic kidney disease, heart failure, stable ischemic heart disease and secondary stroke prevention.
Conclusion
Given the enormous and growing global burden of hypertension, it is clear that all aspects of prevention, detection, treatment, and control must be improved. The significance of accurate blood pressure measurement in hypertension diagnosis and management cannot be overstated. The observer is responsible for a large portion of the error in BP measurement. As a result, it is necessary to simplify, standardise, and automate measuring procedures in addition to ensuring that observers are properly educated, trained, and certified. Even these seemingly simple recommendations can be difficult to implement, but they have the potential to significantly improve hypertension detection and management worldwide. Given the importance of accurate BP assessment and the lack of impact of previous efforts to train healthcare workers, regular certification in BP assessment should be considered.To summarise, the huge disparity between hypertension prevalence and control, both globally and in India, should serve as an important wakeup call that CVD will be a major burden of disease for many years to come, especially if we continue on this path.
References
- Nguyen TN& ChowCK, Global and national high blood pressure burden and control. Lancet.2021 Sep 11;398(10304):932-933.doi: 10.1016/S0140-6736(21)01688-3.
- Kumar V, AgarwalS, Saboo B & Makkar B, RSSDI Guidelines for the management of hypertension in patients with diabetes mellitus. Int J Diabetes Dev Ctries 2022 Dec 15;42(Suppl 1):1-30. doi: 10.1007/s13410-022-01143-7.
- EttehadD,et al. Blood pressure lowering for prevention of cardiovascular disease and death: A systematic review and meta-analysis. Lancet.2016 Mar 5;387(10022):957-967.doi: 10.1016/S0140-6736(15)01225-8.
- Ramakrishnan S,et al. Prevalence of hypertension among Indian adults: Results from the great India blood pressure survey. Indian Heart J. 2019 Jul-Aug;71(4):309-313.doi: 10.1016/j.ihj.2019.09.012.
- Gupta R & XavierD, Hypertension: The most important non communicable disease risk factor in India.Indian Heart J. 2018 Jul-Aug;70(4):565-572.doi: 10.1016/j.ihj.2018.02.003.
- GeevarZ,et al. Prevalence, Awareness, Treatment, and Control of Hypertension in Young Adults (20–39 Years) in Kerala, South India. Front. Cardiovasc. Med.2022 Apr 18; 9:765442. doi: 10.3389/fcvm.2022.765442.
- AnchalaR,et al. Hypertension in India: A systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J. Hypertens.2014 Jun;32(6):1170-7.doi: 10.1097/HJH.0000000000000146.
- https://www.who.int/india/health-topics/hypertension
- Wu CY,et al. High blood pressure and all-cause and cardiovascular disease mortalities in community-dwelling older adults.Medicine (Baltimore). 2015 Nov;94(47):e2160.doi: 10.1097/MD.0000000000002160.
- https://www.who.int/india/news/detail/02-06-2022-india-hypertension-control-initiative–a-high-impact-and-low-cost-solution.
- FuchsFD& WheltonPK, High Blood Pressure and Cardiovascular Disease. Hypertension 285–292 (2020) doi:10.1161/HYPERTENSIONAHA.119.14240.
- Padwal R,et al. Optimizing observer performance of clinic blood pressure measurement: A position statement from the Lancet Commission on Hypertension Group. J. Hypertens.2019 Sep;37(9):1737-1745.doi: 10.1097/HJH.0000000000002112.
- WheltonPK, et al. Harmonization of the American College of Cardiology/American Heart Association and European Society of Cardiology/European Society of Hypertension Blood Pressure/Hypertension Guidelines. Eur. Heart J.2022 Sep 14;43(35):3302-3311.doi: 10.1093/eurheartj/ehac432.
- UngerT,et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension 75.2020 Jun;75(6):1334-1357.doi:10.1161/HYPERTENSIONAHA.120.15026.
- Adler A,et al. Pharmacological blood pressure lowering for primary and secondary prevention of cardiovascular disease across different levels of blood pressure: an individual participant-level data meta-analysis. Lancet 397, 1625–1636 (2021). doi: 10.1016/S0140-6736(21)00590-0.
- ManciaG,et al. 2018 ESC/ESC guidelines for the management of arterial hypertension. J. Hypertens. 25, 2007 Jun;25(6):1105-87.doi: 10.1097/HJH.0b013e3281fc975a.
- KoyaSF,et al. Hypertension control rate in India: systematic review and meta-analysis of population-level non-interventional studies, 2001–2022. Lancet Reg. Heal. – Southeast Asia 9, 100113 (2023).
- Group, SPRINT Research, Jackson T. Wright, Jr., M.D., Ph.D., J. et al. A Randomized Trial of Intensive versus Standard Blood-Pressure Control. N. Engl. J. Med.2015 Nov 26;373(22):2103-16.doi: 10.1056/NEJMoa1511939.
























