Abstract
Climate change is a serious global health concern. Longer allergy seasons and worsening air quality are the results of rising temperatures brought on by climate change. Extreme weather events increased exposure to pollen and other allergens, all contributing to worsening allergy and asthma symptoms with a rising prevalence of allergic disorders. Allergic disorders are conditions induced by the immune system’s hypersensitivity to normally harmless chemicals known as allergens. Allergic diseases include Allergic Rhinitis (AR), allergic asthma, urticaria, atopic dermatitis, contact allergies, and food allergies. The prevalence of allergic illnesses is rising globally, which is quite concerning. AR is the most common of all atopic diseases, afflicting 10%–30% of adults and up to 40% of children all over the world. The increased prevalence of allergic airway disease worldwide can be partially attributed to those global environmental changes. Climate change and air pollution pose adverse impacts on respiratory allergies. The chronic and recurring nature of AR, which results in poor quality of life and work/school loss despite the fact that it is not a life-threatening condition, poses a serious healthcare challenge.
Keywords: Allergic Rhinitis, Asthma, Climate change, Air pollution
Conflict of Interest: Aristo Pharmaceuticals Private Limited, India
Introduction
In 2005 the first World Allergy Day was celebrated. After much deliberation, it was concluded that additional time was needed to accomplish all of the goals of World Allergy Day, and in 2011 World Allergy Awareness Week was created. World Allergy Week, a global initiative of the World Allergy Organisation (WAO), is observed this year from June 18 to June 24 to increase public awareness of allergic disorders and other related medical issues.
There is also a focus on advocating for the provision of training and resources about diagnosis, management, and ways that certain allergies can be prevented. The theme for World Allergy Week 2023 is‘Climate Change Worsens Allergies. Be Ready.’ This year the focus is on managing allergic diseases amidst environmental changes.
Need for Clean Air: Climate Change is Cited as the Cause of Recent Increases in Allergy and Asthma Prevalence
In recent years, it has become increasingly clear how climate change is affecting the environment, biosphere, and biodiversity. Carbon dioxide (CO2) and other greenhouse gases have become more prevalent in the atmosphere due to human activity. With an increased CO2 concentration, plant growth is affected in various ways, leading to prolonged pollination periods. Longer warm seasons result in longer pollen seasons and, therefore, longer allergy seasons.[1] The steady increase in global temperatures, resulting from the combustion of fossil fuels and the accumulation of greenhouse gases (GHGs), continues to destabilize all linked to the rising frequency of respiratory allergic diseases and bronchial asthma.[2]
1 President-Medical & Regulatory Affairs, Dept. of Scientific, Aristo Pharmaceuticals Private Limited, India
Corresponding author: Dr. Manish Maladkar, President-Medical & Regulatory Affairs, Dept. of Scientific, Aristo Pharmaceuticals Private Limited,
India. Email: scientific@aristopharma.co.in
The number of airborne pollutants in the environment has increased as a result of climate change. It impacts the air we breathe by increasing the risk that air pollution, including ozone and particle pollution, will worsen. As temperatures increase, warmer air helps to form ground-level ozone, sometimes called smog, which is a powerful air pollutant. Ozone irritates the lungs which may trigger an asthma attack. Asthma and allergy symptoms can be worsened by mold growth, increasing storms, precipitation, flooding, temperatures, and humidity.[3] In addition to having a considerable negative impact on human health and well-being, air pollution and climate change can also cause or aggravate chronic respiratory disorders including asthma and allergic rhinitis.[4]
Burden of Allergic Rhinitis
Allergic rhinitis is a global health problem. It is the sixth most prevalent chronic disease in the world with approximately 1 million people affected each year including up to 40% of the student population.[5] In India, allergic rhinitis has increasingly become more common during the past 20 years. The prevalence of the disease among adults ranges from 20% to 30%. According to an Indian study, allergic rhinitis was prevalent in children between the ages of 6-7 and 13–14, with a frequency of 11.3% and 24.4%, respectively.[6] People of all ages suffer from AR, a common allergic condition that is usually untreated. Because it is often perceived as just a nuisance, many patients do not seek medical treatment, and others self-medicate with over-the-counter products.[7]
Triggers for Allergic Rhinitis
Currently, more than 25% of India’s overall population has some kind of allergy sensitivity. The most common triggers include dust mites, insects, animal dander, pollen grains, pollution, and food allergens such as milk, egg, soy, wheat, nut, or fish, prawn, almonds, Baker’s yeast, mushroom, ripe mango, rajma, cinnamon, beans, and areca nut. [8,9]
Physical and Mental Symptoms of Allergic Rhinitis
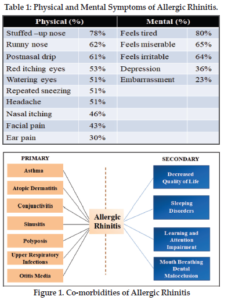
Allergic rhinitis is triggered by various allergens which cause cardinal symptoms such as sneezing, itching, runny nose, and nasal congestion (Table. 1) which is considered as one of the bothersome symptoms causing sleep disturbances. [10,11]
Allergic Rhinitis and Comorbidities: More Than Just a Runny Nose
For both children and adults, AR is more than just sneezing and nose itching. Importantly, AR should be taken into account in the context of systemic allergy illness as it is rarely encountered in isolation. The presence of AR has been associated with numerous comorbid disorders, including asthma, chronic otitis media, rhinosinusitis, oropharyngeal lymphoid hypertrophy, secondary obstructive sleep apnea, and disordered sleep (Figure 1). Poorly controlled AR can trigger exacerbations of these comorbidities because they often share pathophysiologic (inflammatory) pathways in common with AR. Moreover, if left untreated, AR symptoms themselves can worsen, leading to a spiral of worsening comorbidities.[11]
Double-Trouble: Allergic Rhinitis and Asthma
The increased frequency of allergies and asthma in India has become a significant public health concern, with symptoms ranging from mild rhinitis to severe asthma and even life-threatening anaphylaxis. Patients with AR are three times more likely to develop asthma. The CARAS study, an Indian survey reported the co-morbidity of AR in asthma patients with a high incidence of 65.24%.[12]
Social and Psychological Impact of Allergic Rhinitis
When left uncontrolled, AR becomes the dominant factor in patients’ lives, affecting social life, school, sleep, work, and even mental health. In a study group, 79.5% acknowledged that they felt ashamed to communicate with others due to their annoying symptoms which in turn led to difficulty in mingling with peers leading to social disjunction. Complications of this disease are numerous and can have a significant impact, both physically and psychosocially.[5]
Interventions to Modify Air Pollution and Climate Change [4]
While actions of individual citizens can mitigate air pollution only to a small extent, larger lifestyle changes at the population level mainly result from policy interventions.
Lifestyle Adjustments
Various lifestyle adjustments can mitigate air pollution and climate change and indirectly decrease the onset and progression of respiratory diseases.
- At a local level, greenhouse-gas emissions can be reduced by shifting from private motorized transport to more sustainable modalities, such as public
transport, cycling, and walking. - The transition from fossil fuels to renewable energy sources and the industry’s commitment to a full phase-out of coal power are crucial steps on the
road to a more ecologically friendly economy. - Limiting the time spent outdoors during the pollen season (for pollen-allergic patients) and during high-traffic hours or warm days is a reasonable approach.
- Reduce exposures to allergens and air pollutants by staying indoors in air-conditioned environments during air quality alerts and high pollen days.
- If using an air conditioner, be sure to change the filter regularly.
- Wash exposed skin and clothes when returning from outdoors, as pollen can travel on skin and clothes.
- Prevent molds by avoiding damp indoor environments.
Investigations
The key to diagnosing allergic rhinitis is to conduct a comprehensive history, physical and clinical examination.[13] In a patient with suspected AR, the physical examination includes visual assessment for outward signs such as mouth breathing, frequent sniffling or throat clearing, allergic salute or nasal crease. Clinical examination involves anterior rhinoscopy and nasal endoscopy for abnormal secretions, or structural abnormalities. Other assessments include examination of ears, sinus, oropharynx, chest, and skin.
Allergy testing is essential for confirming allergens that trigger rhinitis. Skin-prick testing is considered a reliable method for identifying specific allergic triggers of rhinitis. The use of allergen-specific IgE tests (Blood tests) offers an in vitro measurement of a patient’s specific IgE levels against certain allergens and is a reasonable substitute for skin prick testing.
Differentiating Indicators Between the Common Cold and Allergic Rhinitis
AR is a condition affecting the nose. Due to several common symptoms, including sneezing and a runny nose, it is usually mistaken for the common cold. The main difference between the common cold and AR is the duration of symptoms. If the symptom lasts for more than 2 weeks, regardless of the time of the year it should be an indication of a cause other than common cold infection. In addition, the presence of fever, malaise, and sore throat are more indicative of a common cold. In AR patients, the mucus is clear and watery whereas in common cold, mucus is thick yellow or green. The cause of allergic rhinitis is not a virus, in contrast to the common cold. [14]
Non-Allergic Rhinitis [15]
Although the illness is not due to allergies, non-allergic rhinitis is characterized by recurrent or chronic symptoms that are similar to those of allergic rhinitis. Examples of rhinitis include infectious rhinitis (the common cold), vasomotor rhinitis, hormonal rhinitis, specific types of occupational rhinitis, gustatory and drug-induced rhinitis, non-allergic rhinitis with eosinophilia syndrome (NARES). Cigarette smoke, strong odors, and fumes, including perfume, hair spray, other cosmetics, laundry detergents, cleaning products, pool chlorine, car exhaust, and other air pollution are allergens that can cause vasomotor rhinitis. Cooking spices, alcoholic beverages (especially beer and wine), aspirin, and several medications are additional irritants.
Unmet Needs in AR
Many patients are dissatisfied with their treatment because the symptoms are inadequately controlled, they do not want a lengthy treatment for a condition they perceive as non-threatening, and/or they experience unacceptable side effects.[16]
Need for “Tailored” Therapy for Allergic Rhinitis
Allergic Rhinitis therapy should be tailored based on the severity of the disease, co-morbidities, treatment availability and affordability, and the patient’s preference.[16] Treatment requires a stepwise approach that includes allergen avoidance, pharmacotherapy, and possibly immunotherapy.[8] Relieving symptoms and preventing disease progression and its complications are the primary therapeutic objectives for allergic
rhinitis.[14]
Current pharmacologic options include oral and intranasal antihistamines, intranasal corticosteroids, oral and intranasal decongestants, oral and intranasal anticholinergics, and leukotriene receptor antagonists. The cornerstones of therapy are second-generation
oral antihistamines and intranasal corticosteroids; practice guidelines recommend using intranasal corticosteroids as first-line therapy for moderate to severe allergic rhinitis.[17] Optimal management of rhinitis may improve the symptoms of co-existing asthma especially if it is mild asthma. Combination therapy is indicated in patients with moderate-severe or persistent symptoms of AR. It provides better control over the daytime and night-time symptoms of AR. Also, improves QOL and patient compliance.[18]
Conclusion
Air pollution and climate change have a significant impact on human health and well-being and contribute to the onset and aggravation of allergic rhinitis and asthma among other chronic respiratory diseases. Given the explosive global rise in urbanization, industrial production, aviation, road traffic, etc, the preservation of good air quality will become increasingly challenging. Implementing mitigation strategies to reduce greenhouse gas emissions is critical to prevent further warming of the planet and protect public health. Lifestyle changes, including changes in transportation habits and the use of renewable energy, can help decrease global emissions.
“Don’t Stress. As long as you have breath, you’re blessed”
– Rumi
References
- Gennaro D A, Herberto J C, Olga P M et al. The effects of climate change on respiratory allergy and asthma induced bypollen and mold allergens. Allergy.2020;75(9):2219-2228.
- Pacheco S E, Guillermo G F, Isabella A M et al. Climate change and global issues in allergy and immunology. J Allergy Clin Immunol.2021;148(6):1366-1377.
- Climate Change and Its Impact on Seasonal Allergies. American Lung association.2019.
- Ibon E G, Alexander G M, Sabine B et al. The need for clean air: The way air pollution and climate change affect allergic rhinitis and asthma. Allergy.2020;75(9):2170-2184.
- Kumar K A, Sarun D D, Jeppu A K. Social and Psychological Impact of Allergic Rhinitis among University Students in Malaysia. Indian Journal of Public Health Research &
Development.2020;11(6). - Mamidipudi K T, Padukudru A M, Pudupakkam V et al. An appraisal of allergic disorders in India and an urgent call for action. World Allergy Organ J.2020;13(7):100446.
- Hadley J A, Derebery J M, Marple B F. Comorbidities and allergic rhinitis: Not just a runny nose. The Journal of Family Practice. 2012;61(2):S11-S15.
- Bhattacharya K, Sircar G, Dasgupta A et al. Spectrum of Allergens and Allergen Biology in India. Int Arch Allergy Immunol.2018;177 (3): 219–237.
- Mehta D, Dagar A, Kishan J et al. Common Allergens Prevalent in and Around Ambala, Haryana: An Intradermal Study among Patients with Asthma and Allergic Rhinitis and Atopic Dermatitis. Indian J Dermatol.2018;63(4):311–316.
- Yang-Gi Min. The Pathophysiology, Diagnosis and Treatment of Allergic Rhinitis. Allergy Asthma Immunol Res.2010;2(2):65–76.
- Ruby S, Pawankar, Sanchez Borges et al. The burden of allergic diseases. World Allergy Organization.2011.
- Jaggi V, Dalal A, Ramesh BR, Tikkiwal S, Chaudhry A, Kothari N et al., Coexistence of allergic rhinitis and asthma in Indian patients: The CARAS survey. Lung India.2019;36:411-6.
- Peter S and Harold K. Allergic rhinitis. Allergy Asthma Clin Immunol.2011;7(1): S3.
- Bharrgava S, Sheth K, Bharathi MB, Dabholkar Y, Pendakur A, Desai A et al. Indian guidelines on diagnosis and mangement of Allergic Rhinitis- A consensus approach
- Akhouri S, House S A. Allergic Rhinitis – StatPearls – NCBI Bookshelf.
- Bousquet J, Mondher T, Bernardo S P et al. The Allergic Rhinitis and Its Impact on Asthma (ARIA) Approach of Value-Added Medicines: As-Needed Treatment in Allergic Rhinitis. The Journal of Allergy and Clinical Immunology: In Practice.2022;10(11):2878-2888.
- May J R and Dolen W K. Management of Allergic Rhinitis: A Review for the Community Pharmacist. Clin Ther. 2017 Dec;39(12):2410-2419.
- Xu Y, Zhang J, Wang J et al. The Efficacy and Safety of Selective H1-Antihistamine versus Leukotriene Receptor Antagonist for Seasonal Allergic Rhinitis: A Meta-Analysis. PLoS ONE.2014;9(11): e112815.























