Abstract
Mental health is a barometer of individual productivity and community wellness. It is important both for the people, as well as general and family physicians to be well informed about symptoms, types, and treatment modalities of mental health conditions, as well as remove misconceptions and stigmas attached to some mental health disorders. Awareness and understanding of mental health conditions can enable timely help, referral, and management, to provide a fulfilled life.
Keywords: Mental health, anxiety, depression, mood, psychosis, wellness
Conflict of Interest: None declared
Source of Support: None declared
Introduction
Mental health conditions are an ignored health aspect in society, and associated with myths and stigmas, unlike physical illnesses. Globally, 1 in 8 people live with a mental health disorder at some point in their lives.1 In 2020, estimates showed a 26–28% rise in anxiety-depression in just one year. In India, 14–15% of the population suffers from mental health problems, with more than 50 million people suffering from depression and anxiety disorders.2 Substance abuse is a recognized category of mental disorders, especially in men, with an alarming 25% population prevalence, and can be associated with psychosis, mood, and anxiety disorders.
Health surveys have revealed that 50–60% of people have inadequate awareness, and fixed, adverse opinions of people diagnosed with mental health disorders.3 Often, mental health disorders get clubbed as a single entity in a common person’s mind, but there are many defined types of mental illnesses, treated differently, and specifically (Table 1).
People may go through psychological issues due to circumstances, or emotional stress, for which they may seek medical help, and benefit from treatment.4 On the other hand, a mental health disorder may be dismissed off as a low phase and not diagnosed.5 Mental health disorders are those that fit defined criteria of consistent and significant symptoms and abnormalities in emotions and behaviour, present over a certain period of time, are uncontrollable, and significantly impact personal, social and occupational functioning.6 Mental illnesses can manifest as feeling nervous, sad, swinging moods, social withdrawal, suicidal thoughts, aggression, change in sleep and eating patterns, and relationship problems.7 Sometimes two or more mental disorders can co-exist or even lead to each other.
Types of Mental Health Disorders
Table 1 mentions the 5 most common mental health disorders types that a general or family physician should be familiar with. These include Psychosis, Disorders of Mood, Stress and Anxiety, and Substance Abuse. Apart from these, there are disorders of sleep, and personality disorders. Neurodevelopmental disorders include autism spectrum disorder and attention deficit hyperactivity disorder (ADHD). The complete classification is available in the Diagnostic and Statistical Manual (DSM 5) of Mental Disorders.8
1Chief Editor, The Indian Practitioner, and Medial Director, Dr Varsha’s Health Solutions, Mumbai.
2Psychotherapist and Psychology Counsellor, Mumbai
Table 1. Common mental health disorders.
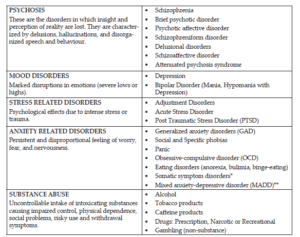
*Though classified separately, are also elaborated under anxiety-related disorders as their causal basis is linked to anxiety.
**It is a diagnostic category defining patients who suffer from both anxiety and depressive symptoms of limited and equal intensity accompanied by at least some physical symptoms and do not meet the criteria for specific anxiety or depressive disorders.
Other disorders include DISSOCIATIVE DISORDERS like dissociative amnesia/fugue, depersonalization/derealization and dissociative identity disorder (formerly called split/multiple personality disorders) are somewhere between the realm of psychosis and disorders of mood, stress, and anxiety.
What Causes Mental Health Disorders?
The following have been some of the causes brought forward by scientific research and medico-social studies:8,9
- Biological factors: Genetic predisposition and family history.
- Brain Development and Physiology: Functioning of the limbic system that regulate emotion, and behaviour, hippocampus (controls learning and memory), and the prefrontal and frontal cortex (controls thoughts, cognition, planning, motivation and actions).
- Neurotransmitters: These include serotonin and noradrenaline (decreased in depression), GABA (decreased in anxiety), glutamate (increased in anxiety), and dopamine (increased in psychosis).
- Hormones: Cortisol and adrenaline increase in stress and anxiety disorders. Other hormones affecting mood are thyroid hormones and oestrogen in women.
- Personality and temperament predisposition: Certain personality types like neuroticism and introversion, and person’s temperament can affect risk of mental health conditions.
- Lifestyle, social, and environmental factors: Many mental health conditions can be traced to underlying unpleasant events, stressors and trauma, especially in childhood. Social and cultural practices, extent of education and family support also play a role.
- Physical health: Underlying physical conditions, poor sleep, diet, and physical activity, may lead to mental health disorders like depression and anxiety.
Holistic Management of Mental Health Conditions
In managing mental health disorders, understanding, support, and cooperation of household members and family is of paramount importance for good and long-term treatment outcomes.
Psychoeducation
This is the first step which involves learning about the condition, its implications in daily life, its impact on the patient and family, and support and treatment options available to help both the patient and family to improve coping and treatment response.
Lifestyle and personal health
This focuses on daily aspects like a nutritious diet with timely meals, regular physical exercise, mindfulness, relaxation and breathing techniques, improving sleep, personal hygiene, and home-social environment, and treating any associated physical illnesses.
Counselling and psychotherapy
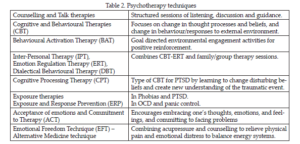
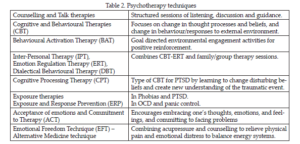
Various techniques of psychotherapy, evolved over a period of timework well on their own, and also enhance the response to medicines, but require patience and commitment.10 Such treatments are usually given by qualified and experienced psychologists and sometimes even by psychiatrists (Table 2).
Medicines and supplements
There are many classes of medications (Table 3) that are effective and have been used in treating mental health disorders.11 These should be prescribed after proper psychiatric evaluation, and under strict medical monitoring of effects and side-effects with regular follow-up.
Nutritional Supplements
There is some evidence to show that certain supplements may help as adjunctive or add-on therapy to improve mental health, like vitamin D, B group vitamins, minerals like iron, zinc, and magnesium, omega 3 fatty acids, melatonin (for sleep), L-theanine, and probiotics. However, more research and conclusive evidence is needed
Other therapies
These include Biofeedback (using visual or auditory feedback to train a person to recognize and control the physical signs of stress and anxiety), Hypnotherapy (to identify and resolve root causes) and Light therapy. Transcranial magnetic stimulation (TMS) is a non-invasive procedure that uses magnetic fields to stimulate specific areas in the brain, in severe and refractory depression.
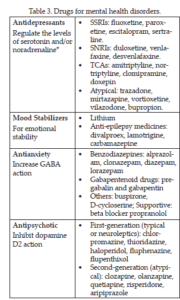
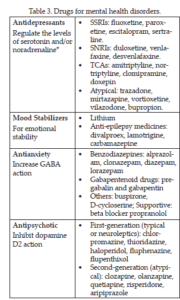
*Selective serotonin reuptake inhibitors (SSRIs); Serotonin and noradrenaline reuptake inhibitors (SNRI); Tricyclic antidepressants (TCA)
Institutionalization or hospitalization (partial/full) in a mental health facility may be needed in some cases that are resistant to most treatments.12
Support groups, helplines, and organizations
There are various support groups, and non-government organizations (NGOs) especially for anxiety-depression, PTSD, and substance abuse for sharing experiences, motivation, and collective commitment. There are also suicide helplines and rehabilitation centres for substance abuse.
Conclusion
Awareness, Acceptance, and Action are the 3 aces of effectively approaching mental health disorders and conditions, and greatly improving an individual’s quality of life and productivity, as well as elevating the level of community health and harmony.
References
- Mental Disorders: Key Facts. World Health Organization (WHO) [Internet]. June 8, 2022. Cited May 12, 2024. Available from https://www.who.int/news-room/fact-sheets/detail/mental-disorders
- Dhyani A, Gaidhane A, Choudhari SG, Dave S, Choudhary S. Strengthening Response Toward Promoting Mental Health in India: A Narrative Review. Cureus. 2022 Oct 18; 14(10): e30435
- TLLLF 2018 Report How India Perceives Mental Health [Internet]. cited May 12, 2024. Available from https://www.scribd.com/document/445093805/TLLLF-2018-Report-How-India-Perceives-Mental-Health
- National Collaborating Centre for Mental Health (UK). [Internet] Common Mental Health Disorders: Identification and Pathways to Care. Leicester (UK): British Psychological Society (UK); 2011. (NICE Clinical Guidelines, No. 123.) 2, COMMON MENTAL HEALTH DISORDERS. Cited May 12, 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK92254/
- Martin-Key NA, Olmert T, Barton-Owen G, Han SYS, Cooper JD, Eljasz P, Farrag LP, Friend LV, Bell E, Cowell D, Tomasik J, Bahn S. The Delta Study – Prevalence and characteristics of mood disorders in 924 individuals with low mood: Results of the of the World Health Organization Composite International Diagnostic Interview (CIDI). Brain Behav. 2021 Jun; 11(6): e02167.
- Sekhon S, Gupta V. Mood Disorder. In: StatPearls [Internet]. May 08, 2023. Cited May 12, 2024. Treasure Island (FL): StatPearls Publishing; 2024 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK558911/
- Diagnostic and Statistical Manual (DSM5) of Mental Disorders. American Psychiatric Association. Cited May 12, 2024. Available from https://www.psychiatry.org/File%20Library/Psychiatrists/Practice/DSM/APA_DSM-5-Contents.pdf
- National Institutes of Health (US); Biological Sciences Curriculum Study. NIH Curriculum Supplement Series [Internet]. Bethesda (MD): National Institutes of Health (US); 2007. Information about Mental Illness and the Brain. Cited May 12, 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK20369/
- Remes O, Mendes JF, Templeton P. Biological, Psychological, and Social Determinants of Depression: A Review of Recent Literature. Brain Sci. 2021 Dec 10; 11(12): 1633.
- Chaimowitz G, Weerasekera P, Ravitz P. Psychotherapy in Psychiatry. Can J Psychiatry. 2021 Nov; 66(11): 999-1004.
- National Institute of Mental Health. Mental Health Medications. Dec 2023. Cited May 12, 2024. Available from https://www.nimh.nih.gov/health/topics/mental-health-medications
- Chow, W.S., Priebe, S. Understanding psychiatric institutionalization: a conceptual review. BMC Psychiatry 2013; 13: 169.























