Hyperacute Outer Retinal Dysfunction (HORD): A Distinct Pediatric Retinal Condition
A multicenter study led by researchers from the State Key Laboratory of Ophthalmology in China has identified a new retinal disorder in children following a high fever illness. This condition, termed hyperacute outer retinal dysfunction (HORD), is characterized by sudden bilateral vision loss, photoreceptor disruption, and variable recovery.
Study Findings: Severe Vision Loss Following Febrile Illness
The study, published in JAMA Ophthalmology, examined eight pediatric patients between the ages of 3 and 7 who experienced sudden-onset severe vision loss approximately two weeks after a febrile illness. Despite initially poor visual acuity, most patients showed significant central vision recovery over the course of a year.
Comprehensive Retinal Imaging and Diagnostic Evaluation
Researchers conducted extensive ophthalmic evaluations and multimodal retinal imaging, including:
- Optical coherence tomography (OCT)
- Color fundus photography
- Ultra-widefield imaging
- Fluorescence angiography
- Fundus autofluorescence
- Electroretinography (ERG)
Genetic and serological testing ruled out inherited retinal diseases and autoimmune conditions. Exclusion criteria included inherited retinal disorders, uveitis, and white dot syndromes.
Clinical Presentation: Severe but Potentially Reversible Vision Loss
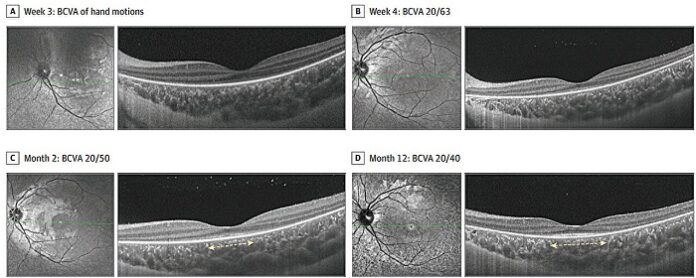
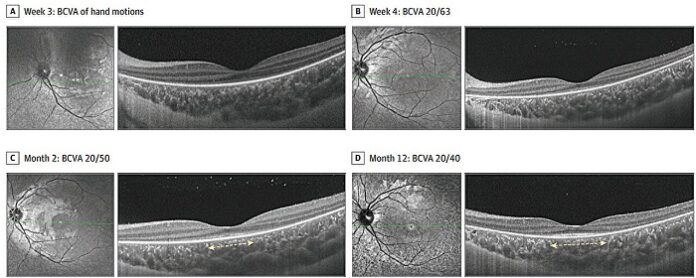
At presentation, all patients exhibited profound bilateral vision loss, nyctalopia, visual field constriction, and dyschromatopsia. The mean best-corrected visual acuity (BCVA) was so poor that patients could not accurately count fingers. OCT imaging revealed extensive ellipsoid zone (EZ) and external limiting membrane (ELM) disruptions, though early fundus examinations appeared unremarkable.
Recovery Patterns and Long-Term Outcomes
By the fourth week, initial signs of macular recovery emerged. After one year:
- 88% (7 of 8 patients) achieved visual acuity of 20/40 or better
- 50% (4 of 8) reached 20/25 or better
- Macular EZ and ELM appeared intact in 75% and 88% of eyes, respectively
- Extrafoveal retinal regions remained affected
However, ERG findings showed persistent loss of rod and cone responses, even in patients with significant visual recovery.
Potential Immune-Mediated Mechanism
As reported by medicalxpress, systemic evaluations did not reveal any clear infectious or autoimmune triggers, though two patients tested positive for specific antiretinal antibodies (antiPKC γ and antiRi). Most patients received corticosteroids, intravenous immunoglobulin (IVIG), or methotrexate, but the study could not determine the definitive effectiveness of these treatments.
Expert Commentary: Possible Autoimmune Etiology
A commentary by Timothy Boyce and Ian Han from the University of Iowa, titled “Hyperacute Outer Retinal Dysfunction—A Retina on Fire,” suggests that HORD may be an inflammatory-mediated retinal disorder. The authors compare its features to autoimmune encephalitis, proposing an antibody-mediated mechanism as a potential cause.
How HORD Differs from Other Retinal Diseases
HORD presents distinct characteristics that differentiate it from other retinal disorders:
- Unlike multiple evanescent white dot syndrome (MEWDS) or acute zonal occult outer retinopathy (AZOOR), HORD causes severe bilateral involvement and only partial recovery.
- Unlike nonparaneoplastic autoimmune retinopathy (np-AIR), HORD affects young children and progresses rapidly.
- Early OCT findings, including vitritis, vascular sheathing, and intraretinal hyperreflective dots, suggest an acute inflammatory response.
Future Directions: Understanding HORD’s Mechanisms and Treatment
Further research is essential to:
- Identify HORD’s underlying etiology
- Determine optimal treatment strategies
- Evaluate long-term prognosis
- Discover specific biomarkers, including potential novel antiretinal antibodies
Understanding these factors could provide valuable insights into disease mechanisms and therapeutic targets, potentially leading to more effective treatments for affected children.






















