A groundbreaking study published in Nature Communications has revealed genetic links between white matter hyperintensities (WMH)—lesions visible as bright white spots on brain MRIs—and cortical thinning, a key feature in dementia.
Researchers from Université de Montréal (UdeM), in collaboration with international partners in the CHARGE Consortium, found that WMH, commonly seen in older adults, are strongly associated with reduced cortical thickness, shedding light on their role in cognitive decline and dementia risk.
“WMH are often seen in older individuals and have been suspected to relate to structural brain abnormalities. We aimed to uncover whether genetic factors could explain their link to cortical atrophy and dementia risk,” said co-lead researcher Zdenka Pausova, a UdeM professor of pediatrics and scientist at CHU Sainte-Justine research center.
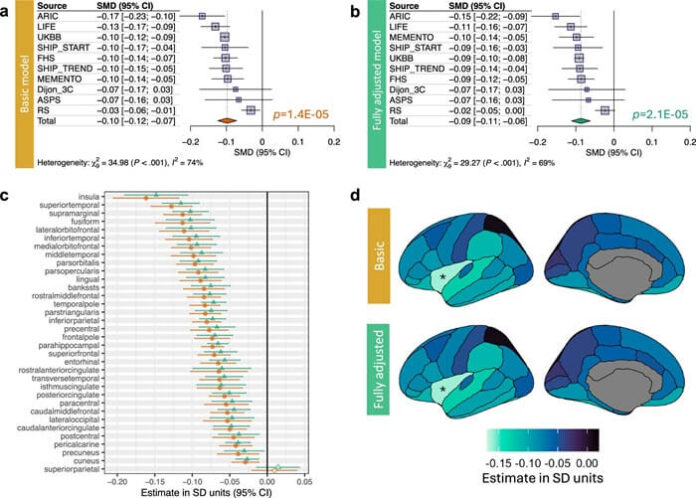
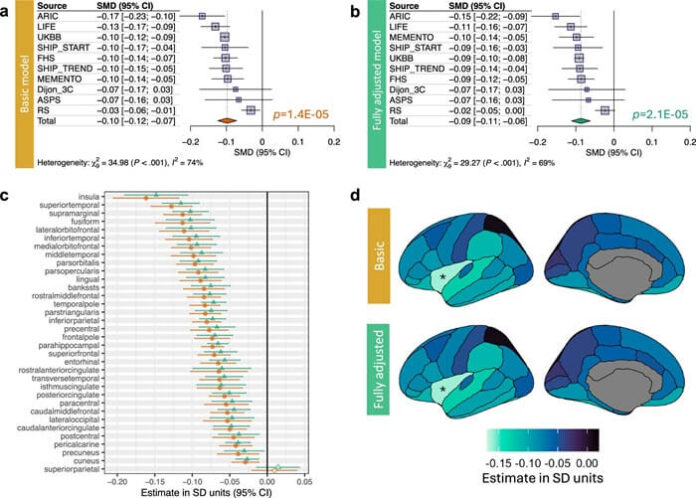
As reported by medicalxpress, the study analyzed data from over 51,000 participants of European ancestry, aged 19 to 100, across 10 cohorts. Researchers consistently observed that higher WMH volume correlated with lower cortical thickness, even after adjusting for vascular risk factors like hypertension and diabetes.
The strongest association was noted in the insula, a critical brain region involved in sensory, emotional, and cognitive functions.
To understand the genetic basis of this relationship, the researchers conducted a genome-wide association study (meta-GWAS), identifying 20 significant genetic loci. Of these, 15 influenced genes critical for axonal transport and cytoskeletal organization, essential processes for neuronal health.
These genetic signals were also enriched in vascular and support cells like astrocytes and oligodendrocytes, reinforcing the theory that vascular health and axonal integrity are key contributors to cortical thinning.
Using their genetic findings, the team developed a polygenic risk score, which was applied to data from 500,000 individuals in Finland. Results showed that higher genetic susceptibility to WMH-related cortical thinning increased the risk for both vascular dementia and all-cause dementia.
“This underscores the importance of vascular health in understanding dementia and highlights the genetic factors that predispose some individuals to this risk,” said Tomas Paus, co-lead author and UdeM neuroscience professor.
The study’s findings provide critical insight into how brain lesions and vascular health influence dementia, paving the way for new approaches to understanding and potentially mitigating cognitive decline.























