India sees 17,000–18,000 solid organ transplants performed every year, the most in the world after the USA and China, but remains behind several high-income countries in transplantation rates per million population (0.65). There has been progress in this area, such as an improvement in the harvesting of organs from deceased donors, with the average number of organ transplants per donor increasing from 2.43 in 2016 to 3.05 in 2022. (Lancet Reg Health Southeast Asia. 2024 Feb 9;21:100366).
The key is to raise awareness of organ donation at the level of both physicians and the community. World Organ Donation Day is observed globally on 13th August.Here we present a Q&A session with Dr. Anil Kumar (Director, NOTTO) and Dr. Atul Goel (DGHS, NOTTO) to address many important points and common queries on organ donation.
Q.1 What is the first point of contact and step if a person wishes to be an organ donor? Are there any pre-donation evaluations and tests that potential donors must undergo?What are the common medical conditions or factors that might disqualify someone from being a donor?
Ans. The first point of contact can pertain to any of the following three situations:
(i) person who wants to be a donor after his death : If a living person wishes to be an organ donor, after death, he/she can register his/her wish on the web-portal www.notto.abdm.gov.in which is Aadhaar verified pledge and for any facilitation and information regarding this, the person may contact NOTTO 24*7 helpline number 1800114770. If family of a deceased brain stem death person wants to donate the deceased person’s organ/s then the doctor on duty in the ICU is the first point of contact or ideally that doctor on duty is required to make enquiry and request the family of a potential organ donor in the ICU.
(ii) person wants to donate as a living donor to a pre-identified recipient: The treating doctor in the hospital is the first point of contact, and will advise for transplant and refer the case to competent authority, in case of a near relative donor, or to the authorization committee in case of other than near relative, foreigner or swap donor.
(iii) person wants to donate as a living altruistic donor to any one, i.e. the recipient is not pre-identified: There is no mechanism in place for this in India at present.
Pre-donation evaluations and tests is done in case of potential living donors.
The evaluation of the donor is usually done by a multidisciplinary team. The goal of the evaluation is to certify the fitness of the donor to undergo the surgery. It is usually a multi-step process which evaluates the patient as follows:
- Basic tests for the general health of the patient.
- Tests specific to the concerned organ to evaluate for surgical compatibility.
- Tests for other organ systems of the body
- Evaluation of fitness for general anesthesia.
Common medical conditions or factors that might disqualify someone from being a donor are as follows:
Absolute Exclusion Criteria
- Age <18 years
- Hypertension in someone younger than 50 years old, evidence of end organ damage, or onthree or more anti-hypertensive medications
- Diabetes (diagnosis of diabetes) or abnormal glucose tolerance test
- History of thrombosis or embolism
- Psychiatric contraindications
- Obesity: BMI >35 kg/m2
- Coronary artery disease orsymptomatic valvular disease
- Peripheral Vascular Disease
- Chronic lung disease with impairment of oxygenation or ventilation
- Recent malignancy, or cancer with long times to recurrence e.g., breast cancel
Significant urologic abnormalities of donor kidney
- Proteinuria > 300 mg/24 hours
- HIV infection
Relative contraindications:
- Hepatitis C Virus Infection
- Hepatitis B Virus Infection
- Age 18-21 years old; elderly donors especially those without significant comorbid disease
- Obesity (BMI 30-35)
- Kidney stones
- Distant history of cancer
- Past history of psychiatric disorder
- Renovascular disease
- Thin basement membrane disease
- Prior valve surgery
- Moderate cardiac valvular disease with otherwise normal echocardiographic findings
- Mild sleep apnea without pulmonary hypertension
DECEASED DONOR
Kidney Transplant Contra-indication criteria
- Chronic renal disease
- Age >70 years; can be accepted if other parameters are normal.
- Potential metastasizing malignancy
- Severe hypertension
- Current intravenous abuse
- HIV positive
- Oliguric acute renal failure
- Untreated bacterial sepsis
- Juvenile onset diabetes
Liver Transplant Contra-indication criteria
- HIV
- Malignancy other than primary brain and non-malignant skin tumors
- Organs may also be rejected after assessment of the retrieval surgeon for
- Fatty liver
- Size mismatch
- Significant intrahepatic cholestasis
- Changes of cirrhosis, etc.
Q.2 What are the different organs that can be donated for transplant after death, and what is the critical timing of obtaining them from the donor?
Ans. 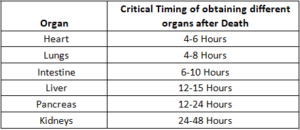
Q.3 Which organ and organ parts can be donated while alive? What are the key medical criteria for determining whether a person is eligible to be a live donor, and what are the advantages to the recipient and risks to the donor in live organ donation?
Ans. Organ and organ parts that can be donated while alive include:
- One kidney: The kidney is the most commonly donated organ. As kidneys are paired organs, one of the kidneys can be donated while alive. The remaining kidney removes waste from the body.
- Part of liver: From a surgical point of view, the liver is divided into right and left lobes in almost a 60:40 proportion by size, by a major fissure. The liver can also be divided into 8 segments.
Depending upon the age, weight, and size of recipient, the volume of liver required varies. Usually for an adult one of the two lobes or in pediatric cases, a segment of the liver can be donated. Remaining liver cells grow to its original size.
- One lobe of the lung, part of the pancreas, or part of the intestine can also be donated. While these organs don’t regrow, the donated portion and the portion that remains can function fully. However, these donations are rare.
The key medical eligibility criteria for a person to be a live donor isa healthy individual of age 18 years and above with no contraindications to donation as mentioned in answer 1.
The advantages to the recipient in live organ donation are:
- Reduced waiting time for an organ transplant. Thus, living kidney donation can prevent—or shorten—the need for kidney dialysis.
- Research has shown that recipients of kidney from living donors have better outcomes than those who receive organs from deceased donors.
- Usually Living donor transplant is done as an elective surgery, hence proper screening of living donor to assess suitability and matching of donor and recipient is feasible due to the adequate time.
- Even in emergency situation of recipient, living donor can be available for saving life.
- There will be very short ischemia time of organ transplanted, so outcome of transplant is expected to be better
The risks to the donor in live organ donation are:
- Inherent risks and complications associated with the surgery including risk of mortality. These risks differ depending on each individual donor as well as the type of organ donated. Short-term effects may include pain or infection from the procedure. Long-term effects can include hypertension for kidney donors, or intestinal problems for liver donors.
- They will require follow up after donation.
- They are declared medically unfit in some of the government jobs.
- living donors have had problems keeping insurance coverage at the same level and rate.
- Loss of wages for being out of work during the recovery period.
Q.4 What protocols are in place to ensure the safety and ethical consideration in organ donation?
Ans.
- The Transplantation of Human Organs& Tissues Act 1994and rules thereunder provide for regulation of the removal, storage and transplantation of human organs and tissues for therapeutic purposes and for the prevention of commercial dealings in human organ and tissues.
- No Hospital is allowed to perform organ retrieval and transplantation without registration which is granted by the state appropriate authority. This authority is also empowered to investigate illegal activities related to transplantation and take actions like issue of notices and cancellation of registration. The authority is also required to inspect hospitals for quality of transplantation and follow up medical care of both donor and recipient.
- All transplant hospitals need to register themself with NOTTO and provide data related to both deceased and living donor transplantations.
- NOTTO under Central Government maintains a national registry wherein the hospitals register the potential recipients of any age from any part of the country and no fee is charged for it. A unique NOTTO id is then generated for each patient and donor which is nationally valid. The registry helps in monitoring the transplantation activities in the country.
- Authorization Committee, a seven-member bodygives permission of live organ donation in case of other than near relative, foreigner patients and swap donation cases. The near relative donor cases are approved at the level of treating hospital’s competent authority.
Q.5 During post death organ donation, who and how is consent taken and what are the legal requirement with respect to attending doctors in-charge of the case, as well as family members?
Ans. In case of a potential Brain Stem Death patient, it is required by the RMP/ICU Doctor to inquire and request for Organ Donation. The doctor is required with the help of the transplant coordinator, if available, to explain the opportunity of organ and tissue donation and encourage the family members of the potential donor. The consent is taken in Declaration cum consent form No. 8 as prescribed under The Transplantation of Human Organs & Tissues rules, 2014.
Near Relative of the deceased person in legal possession of the body can give consent for organ donation.