Abstract
PCOS presents commonly in women of reproductive age group. Its pathogenesis has been studied over decades, and the knowledge is still evolving. Insulin resistance and androgen excess, and the resulting hormonal imbalance presenting as ovulation, menstrual irregularities and infertility, influenced by obesity, diet, lifestyle, metabolic factors, stress, and environmental factors suggest a multifactorial process. Understanding the same can enable effective management with lifestyle and diet solutions, and appropriate medicines and supplements.
Key words: PCOS, insulin resistance, androgen excess, menstrual irregularities, hormonal imbalance, ovulation, infertility.
Introduction and Pathophysiology
Polycystic ovary syndrome (PCOS) is one of the most common endocrine and metabolic disorders in premenopausal women. September is observed as PCOS awareness month globally. PCOS presents with signs and symptoms of androgen excess and ovarian dysfunction.1Hyperandrogenism inhibits follicular development, that can lead to immature oocytes, absence of egg release (anovulation), menstrual abnormalities like oligomenorrhea or amenorrhea, and development of cysts in the underdeveloped follicles. The prevalence of infertility in women with PCOS can be as high as 70-80%, with almost 80% of anovulatory infertility being due to PCOS.2Androgen excess (hyperandrogenaemia) leads to female hormonal imbalance (increase in the luteinizing hormone LH to follicular stimulating hormone FSH ratio), and also leads to acne and hirsutism.3
PCOS affects 5% to 10% of females in the reproductive agegroup. Studies from India have shown prevalence rates of 9-18% in young adolescent females, with up to 22.5% in urban women.4More and more evidence suggest that multiple factors are involved in the etiology and pathogenesis of PCOS that can range from insulin resistance and hyperinsulinemia, obesity, diet and lifestyle, metabolic factors, stress, and environmental influences. Women with PCOS are at an increased risk of developing metabolic syndrome, type II diabetes mellitus, abnormal lipoprotein levels (hyperlipidemia), and cardiovascular disease.5
Apart from the problems of infertility and menstrual abnormalities, and cosmetic issues of acne and facial hair, PCOS is often associated with psychological issues like anxiety and depression. Almost 25-35% PCOS patients show anxiety, depression or both. In comparison to non-PCOS counterparts, the prevalence of depression in PCOS was considerably higher in the overweight and obese categories (PCOS 33.2% vs. non-PCOS 16.2%; P < 0.001).6
There is a high incidence of insulin resistance in PCOS patients independent of obesity, and insulin resistance is a major mechanism and now considered the central factor in developing PCOS, its clinical symptoms and other metabolic complications.7 Resistance to insulin leads to an increase in androgen production, increased free testosterone availability, reduced sex hormone binding globulin (SHBG), and increased blood insulin level. (Figure 1)8.
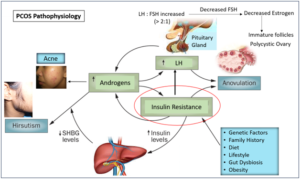
LH: Luteinizing Hormone; FSH: Follicle Stimulating Hormone; SHBG: Sex Hormone Binding Globulin
Figure 1: PCOS Pathophysiology
Chronic gut inflammation and gut dysbiosis are also now postulated to contribute to both insulin resistance and PCOS. Gut microbiota deficiency is associated with disorders of lipid, glucose, and steroid hormone metabolism, and studies have demonstrated that gut microbiota could regulate the synthesis and secretion of insulin, produce short chain fatty acids (SCFA) that reduces gut inflammation, produce brain gut peptides, and affect androgen metabolism and follicle development.9
Management Approach
Lifestyle modification
There is a renewed interest towards natural therapies in India to treat PCOS holistically and minimize drug related side effects and tolerability issues.10 Diet and lifestyle modification are cornerstones of management along with gradual controlled weight reduction to attain a healthy body mass index (BMI). Drastic fasting or crash diets, sudden intense weight loss, and unsupervised severe exercise should be avoided. Meals should be healthy with more vegetables, fruits, curd, whole grains, and proteins, and low on refined carbohydrates and sugar. Appropriate physical activities like brisk walking, swimming, aerobics, etc. preferably by a trainer or approaches like yoga are helpful.11 Such modifications also help reduce cardiovascular risk. Stress, PCOS and psychological issues are intricately linked, and therefore stress management, and counselling/psychotherapy should form an integral part of holistic PCOS management.12 Medical treatment of PCOS comprises of agents that improve insulin sensitivity as the central focus along with appropriate hormonal therapy to attain regular menses and ovulation.
Managing insulin resistance
Therapies to address insulin resistance like the most well-known metformin (MET) as well as inositols (myoinositol– MI) act as insulin sensitizers by restoring the diminished GLUT-4 protein levels and cellular glucose uptake in PCOS. MI also exerts its insulin-sensitizer effects by metabolism and generation of Phosphatidylinositol (4,5)-bisphosphate (PIP2) and Phosphatidylinositol (3,4,5)-trisphosphate (PIP3) that act as a second messenger in the insulin pathway through the activation of the enzyme phosphatidylinositol-3-kinase/protein Kinase B (PI3K/AKT).13 Therefore, the insulin sensitizing action of metformin will be limited when deficiency of inositols is present.D-chiro-inositol (DCI), accelerates the dephosphorylation of glycogen synthase and pyruvate dehydrogenase, the rate limiting enzymes of non-oxidative and oxidative glucose disposal. The presence of abnormal ovarian ratios of myo-inositol (MI) to D-chiro-inositol (DCI) is seen in PCOS due to hyperinsulinemia, and elevated DCI causes increased androgen production and poor reproductive outcomes.14 Therefore DCI should be given only with MI in a 40:1 ratio of MI: DCI for maximum benefit.15 Pre-probiotics supplements are now being explored for their potential benefits as they increase the levels of beneficial bacteria like Lactobacilli and Bifidobacteria and also help reduce chronic gut inflammation and insulin resistance. Alpha lactalbumin a prebiotic, acts by both improving gut microbiota as well as increasing the absorption of inositols, so is beneficial as a combination with MI and DCI.16
Hormonal therapy
Hormonal therapy in PCOS is based on the woman’s desire for pregnancy at consultation. Those not desirous of pregnancy are given oral contraceptives (OCPs) for normalizing cycles. Estrogen content in the combination pill increases SHBG levels, thus decreasing the free circulating androgens. The progestin component suppresses the secretion of LH and decreases androgen production and action by competing for 5 alpha-reductase and the androgen receptor.17Combination pills that contain both estrogen and progest in help lower risk of endometrial cancer and correct irregular bleeding, excess hair growth and acne. Menstrual irregularity gets corrected immediately, but acne and hirsutism may take a minimum of 6 months for its effects to be seen. Therefore, topical acne treatment with retinoids and/or antibiotics maybe recommended along with cosmetic removal of facial hair. Counselling regarding the side effects such as weight gain, loss of libido or mood changes, breakthrough bleeding, nausea, and breast tenderness with contraceptives is important. It is also important to discuss the interactions of OCPs with anticonvulsants, antibiotics, benzodiazepines, paracetamol, morphine, and clofibrate. Women who are at risk of CVD, older age, presence of diabetes, hypertension, and dyslipidemias, who are obese, and who smoke should be counselled about the increased risk of CVD.17 Low dose progestin only pills can help with heavy or painful periods, are less likely to cause side effects than combination pills, so can be the option for those with cardiovascular risk.
Those desirous of pregnancy are treated with ovulation inducing agents like letrozole or clomiphene, and gonadotropins, with consideration and planning of in-vitro fertilization in required cases.2,18The first-line pharmacological treatment for inducing ovulation consists of letrozole for timed intercourse. The second-line pharmacological treatment includes the administration of exogenous gonadotrophins mainly as recombinant FSH, as the body has enough LH in the system. Ovulation induction using letrozole and gonadotropins is effective with cumulative live birth rates of approximately 70% and is the most preferred line of treatment currently.19 Ovarian drilling should be performed when laparoscopy is indicated (typically effective in approximately 50% of cases). The third line treatment is, in vitro fertilization (IVF) or intracytoplasmic sperm injection is recommended when the previous interventions fail. IVF is also the first choice in cases of bilateral tubal occlusion or semen alterations that impair the occurrence of natural pregnancy.
Conclusion
PCOS presents commonly in women of the fertile age group. It has been studied to have a multifactorial pathophysiology with centers around insulin resistance, androgen excess, hormonal imbalance and menstrual irregularities, that lead not only to infertility but also cosmetic concerns, psychological issues and increased cardiometabolic risk. Family history, obesity, diet, lifestyle, metabolic factors, stress, gut dysbiosis and environmental factors are contributory factors. Understanding the same can enable effective and holistic management of PCOS with lifestyle and diet solutions, appropriate medicines and supplements.
References
- Escobar-Morreale HF. Polycystic ovary syndrome: definition, aetiology, diagnosis and treatment. Nat Rev Endocrinol. 2018 May;14(5):270-284.
- Sawant S, Bhide P. Fertility Treatment Options for Women with Polycystic Ovary Syndrome. Clin Med Insights Reprod Health. 2019 Dec 27;13:1179558119890867.
- Ndefo UA, Eaton A, Green MR. Polycystic ovary syndrome: a review of treatment options with a focus on pharmacological approaches. P T. 2013 Jun;38(6):336-55.
- Ganie MA, Vasudevan V, Wani IA, Baba MS, Arif T, Rashid A. Epidemiology, pathogenesis, genetics & management of polycystic ovary syndrome in India. Indian J Med Res. 2019 Oct;150(4):333-344.
- Ali AT. Polycystic ovary syndrome and metabolic syndrome. CeskaGynekol. 2015 Aug;80(4):279-89.
- Xing L, Xu J, Wei Y, Chen Y, Zhuang H, Tang W, Yu S, Zhang J, Yin G, Wang R, Zhao R, Qin D. Depression in polycystic ovary syndrome: Focusing on pathogenesis and treatment. Front Psychiatry. 2022 Aug 31;13:1001484
- Shirazi, F.K.H., Khodamoradi, Z. &Jeddi, M. Insulin resistance and high molecular weight adiponectin in obese and non-obese patients with Polycystic Ovarian Syndrome (PCOS). BMC EndocrDisord2021:21:
- Polycystic Ovary Disease. WAOCP [Internet]. Published Nov 29, 1899 (updated 2017), Cited Aug 28, Available from http://waocp.com/journal/index.php/apjcb/article/view/206/1070
- Sun Y, Gao S, Ye C, Zhao W. Gut microbiotadysbiosis in polycystic ovary syndrome: Mechanisms of progression and clinical applications. Front Cell Infect Microbiol. 2023 Feb 24;13:1142041.
- Pandya MR,Khandheria K, Golwala D. Evaluation of clinical efficacy and safety of Ovaryl tablet anherbalformulation in Poly Cystic Ovarian Syndrome (PCOS). Indian Journal of Obstetrics and Gynecology Research, April-June 2015;2(2):73-91.
- Cowan S, Lim S, Alycia C, Pirotta S, Thomson R, Gibson-Helm M, Blackmore R, Naderpoor N, Bennett C, Ee C, Rao V, Mousa A, Alesi S, Moran L. Lifestyle management in polycystic ovary syndrome – beyond diet and physical activity. BMC EndocrDisord. 2023 Jan 16;23(1):14.
- Salajegheh Z, Ahmadi A, Shahrahmani H, Jahani Y, Alidousti K, NasiriAmiri F, Salari Z. Mindfulness-based stress reduction (MBSR) effects on the worries of women with poly cystic ovary syndrome (PCOS). BMC Psychiatry. 2023 Mar 21;23(1):185.
- Cabrera-Cruz H, Oróstica L, Plaza-Parrochia F, Torres-Pinto I, Romero C, Vega M. The insulin-sensitizing mechanism of myo-inositol is associated with AMPK activation and GLUT-4 expression in human endometrial cells exposed to a PCOS environment. Am J PhysiolEndocrinolMetab. 2020 Feb 1;318(2):E237-E248.
- Unfer V, Dinicola S, Laganà AS, Bizzarri M. Altered Ovarian Inositol Ratios May Account for Pathological Steroidogenesis in PCOS. Int J Mol Sci. 2020 Sep 28;21(19):7157.
- Nordio M, Basciani S, Camajani E. The 40:1 myo-inositol/D-chiro-inositol plasma ratio is able to restore ovulation in PCOS patients: comparison with other ratios. Eur Rev Med Pharmacol Sci. 2019 Jun;23(12):5512-5521.
- Pandya MR, Pandya NM, Narayanan V, Adroja KS, Patel VC. Observational study of the usage of a combination of inositols with alpha-lactalbumin (Ovamystic) in the treatment of menstrual irregularity in PCOS.Indian Journal of Obstetrics and Gynecology Research.Nov 2023;10(4):488-493.
- Shah D, Patil M; National PCOS Working Group. Consensus Statement on the Use of Oral Contraceptive Pills in Polycystic Ovarian Syndrome Women in India. J Hum Reprod Sci. 2018 Apr-Jun;11(2):96-118.
- Melo AS, Ferriani RA, Navarro PA. Treatment of infertility in women with polycystic ovary syndrome: approach to clinical practice. Clinics (Sao Paulo). 2015 Nov;70(11):765-9.
- Pandya MR, Patel K . A study of comparison of effectiveness of letrozole (5mg) versus Clomiphene citrate (100 mg) for ovulation induction among infertile women. Indian Journal of Obstetrics and Gynecology Research 2021;8(4):553–558
1Professor and HOD, Obstetrics and Gynecology, Mahavir Hospital, and Manish IVF Center, Surendranagar, Gujarat.
2Chief Editor, The Indian Practitioner, and Medial Director, DrVarsha’s Health Solutions, Mumbai.