Nearly half of the global population is at risk for malaria, with children and pregnant women being the most vulnerable to severe illness and mortality. Current detection methods rely on invasive blood samples, each with limitations that affect their practicality.
In a groundbreaking study published in Nature Communications, Yale School of Public Health epidemiologist Dr. Sunil Parikh, along with collaborators from Cameroon and the University of Arkansas for Medical Sciences, unveils a new noninvasive test that could revolutionize malaria detection, especially in low- and middle-income countries heavily impacted by the mosquito-borne disease.
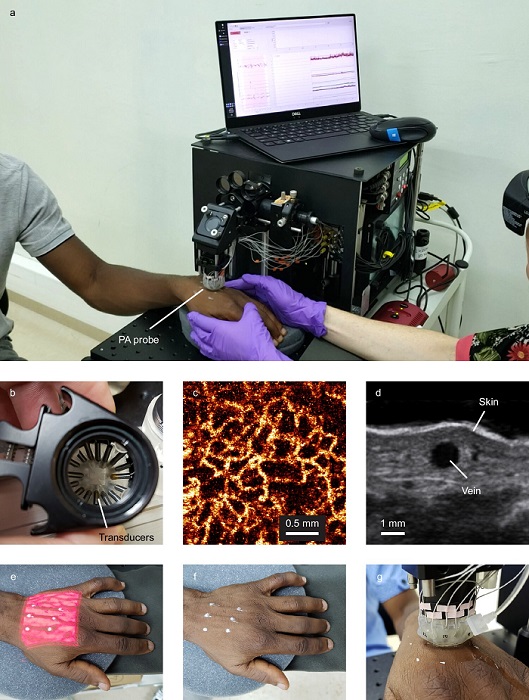
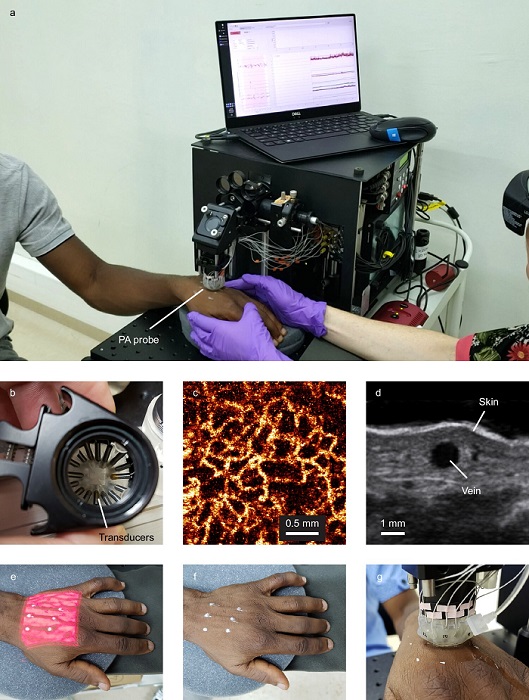
Remarkably, this new test detects malaria without a single drop of blood. Using a device known as the Cytophone, which utilizes targeted lasers and ultrasound, the test identifies malaria-infected cells directly in the bloodstream, explained Jillian N. Armstrong, former Ph.D. student in Parikh’s lab and a lead author on the study. The Cytophone, about the size of a tabletop printer, identifies malaria infection within minutes through a small, noninvasive probe placed on the back of the hand above a targeted vein.
As reported by medicalxpress, the Cytophone’s innovation lies in its ability to detect hemozoin, an iron crystal by-product that accumulates in red blood cells infected by malaria parasites. When exposed to the device’s laser, these hemozoin nanocrystals heat up, giving them unique magnetic and optical properties that the Cytophone detects.
In a study involving 20 malaria-positive adults in Cameroon, the Cytophone achieved 90% sensitivity and 69% specificity, matching and even exceeding the current gold standards for malaria testing, which require blood samples. “Our study showed that the Cytophone was safe and had diagnostic performance comparable to current point-of-care options, using highly sensitive quantitative PCR as the benchmark,” Armstrong said.
The Cytophone was initially developed by bioengineer Dr. Vladimir P. Zharov and his team at the University of Arkansas to detect circulating melanoma cells, but they adapted the technology for malaria detection, with Zharov and Parikh co-leading the study. The device successfully detected Plasmodium falciparum, the deadliest malaria parasite, as well as other less common species, and showed sensitivity in tracking decreases in parasite levels post-treatment.
Parikh and Armstrong praised their Cameroonian colleagues, particularly Professor Yap Boum II, for their crucial role in testing the Cytophone during the COVID-19 pandemic, even when international team members were unable to be present.
The research team plans to enhance future Cytophone models, aiming for greater sensitivity, portability, and possibly battery-powered operation. Malaria remains a significant health crisis, with over 250 million cases and 600,000 deaths annually. The World Health Organization aims to reduce malaria cases by 90% and eliminate the disease from 35 countries by 2030. Cytophone technology presents a promising diagnostic tool to help reach these ambitious goals by improving early malaria detection and enabling faster treatment.






















