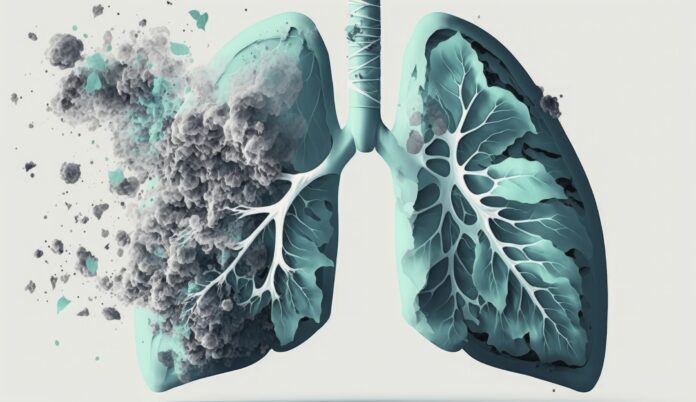
A new study from the Sylvester Comprehensive Cancer Center at the University of Miami Miller School of Medicine has scrutinized the cost-effectiveness of durvalumab, a targeted immunotherapy for lung cancer known to extend patients’ lifespans. Despite its clinical effectiveness, the study found that durvalumab exceeded official cost-effectiveness thresholds in the United States, Brazil, Singapore, and Spain.
Cost-effectiveness analyses are essential for national healthcare systems and insurance companies to balance treatment costs with health benefits. This often restricts access to expensive, yet effective, new therapies. The study’s findings suggest that current pricing structures may limit the number of patients who can benefit from durvalumab, highlighting the need for strategic drug pricing to alleviate financial burdens.
Senior author Dr. Gilberto Lopes emphasized that such analyses could help establish value-based pricing, facilitating discussions with payers and informing biopharma companies about access barriers, potentially leading to adjusted pricing structures.
The study, published in the Journal of the American Medical Association Open Access, utilized a model assessing treatment costs and health benefits over a decade. The U.S. cost of durvalumab treatment was found to be $114,394, with a cost-effectiveness ratio of $228,788 per quality-adjusted life year (QALY), exceeding the $150,000 threshold typically used by Medicaid and Medicare.
In Brazil, despite approval in 2020, durvalumab remains unreimbursed by the public health system. The study highlighted how discounted pricing programs, like those in Singapore, could significantly improve cost-effectiveness, reducing the ratio from $153,461 to $45,164 per QALY.
The researchers concluded that, globally, durvalumab remains “cost-prohibitive” but suggested that reduced pricing could enhance accessibility. The study’s scope included multiple therapy lines and biomarker-guided treatments, but noted limitations such as its narrow global coverage and lack of analysis in poorer countries.
As reported by News Medical, this research underscores the complexity of balancing drug development costs with patient access, a challenge highlighted by Dr. Lopes and echoed by recent industry initiatives to improve treatment availability in low- and middle-income countries.