Summary
The persistent high prevalence of anemia in the Indian population is likely to be a major health hazard. Since mild or moderate anemia is often undetected or uncared for, it results in an imperceptible or unrecognized poor quality of life. It increases the risk to health and to life in many cases. This short review is meant to highlight the unsuspected prevalence, and unperceived effects of anemia in the life of millions of Indians. The national health programs cannot succeed to the desired extent unless healthcare providers understand the nature of anemia and the role of iron supplements. This write up is meant to implore all the healthcare givers and the society at large to relook into the health of the community after relinquishing the lower standards of hemoglobin, and to highlight the importance of being watchful for anemia as an associated or primary cause of illness, a multifactorial malady and to start investigating and treating it with due zeal that the Indian population deserves. We hope that with renewed enthusiasm for detection and management of anemia, the health and performance indicators of India will show a respectable increase. The health of a nation is its wealth!
Introduction
The 5th Family Health Survey by the Government of India is a wakeup call for all physicians, paramedical professionals and policy makers. India has had a National Policy for treatment of Iron Deficiency Anemia (IDA) for more than five decades now. Yet it is observed that more than 50% of women (1 in 2) and 20% of men (1 in 5) are anemic. Given the population of this country, India probably has the highest prevalence of anemia in the world. [1,2,3]
What are the consequences of untreated anemia? What is it that plagues IDA management? Are any solutions possible?
Almost all medical practitioners are aware of the complexities of problems due to anemia but there is an urgent need to take a fresh look. Every patient who approaches the practitioner deserves to be given the necessary attention and care, or referral that is due to the patient. The role of micronutrients i.e., folate, B12 and vitamin A, riboflavin as well as protein cannot be overlooked. It is estimated that in only about 50% of the women, can the anemia be attributed to iron deficiency, while in the other half, anemia is caused by other factors. Tuberculosis, worm infestation, hemorrhoids and diseases of hemoglobin synthesis are other common causes, and in pregnant women, anemia could pose major problems for the mother and fetus during the antenatal and postnatal periods. The main emphasis of most National Health plans is on nutritional iron deficiency and iron supplements (IS).
The Government of India has formulated an excellent policy and treatment guidelines with a training tool kit for use at the national level.[4] This includes Tripartite Government-Public-Private Partnerships and accountability for the health care providers at all levels of management. Digital Hemoglobinometers are to be provided and training is to be given to the users. Appropriate iron and folic acid supplements are described for different ages. Women undergoing pregnancy and lactation and the section of deworming also is linked with this. Under the Intensive National Iron Plus Initiative, the Government of India recommends oral and if necessary parenteral iron preparation, folate and albendazole for prevention and treatment of maternal anemia. Additionally, food fortification and food diversity through inclusion of a variety of foods are promoted as a strategy. Pregnant women are generally prescribed folic acid supplements, but vitamin B12 cannot be neglected. The counseling for women should also include intake of vitamin A/ beta carotene (sources are yellow-orange fruits and vegetables and green leafy vegetables) and riboflavin in their diets. Vitamin B12, vitamin C, vitamin E, zinc, and copper are also important.
Anemia is also likely to be caused by non-nutritional factors like hemoglobinopathies or other enzyme defects or hemolysis that occurs in malaria. When these are missed, patients do not respond to the routine treatment. Additionally, they are already likely to have unutilized iron in circulation and the addition of extra iron through IS will very likely cause side effects; in some cases, this may amount to iron overload.
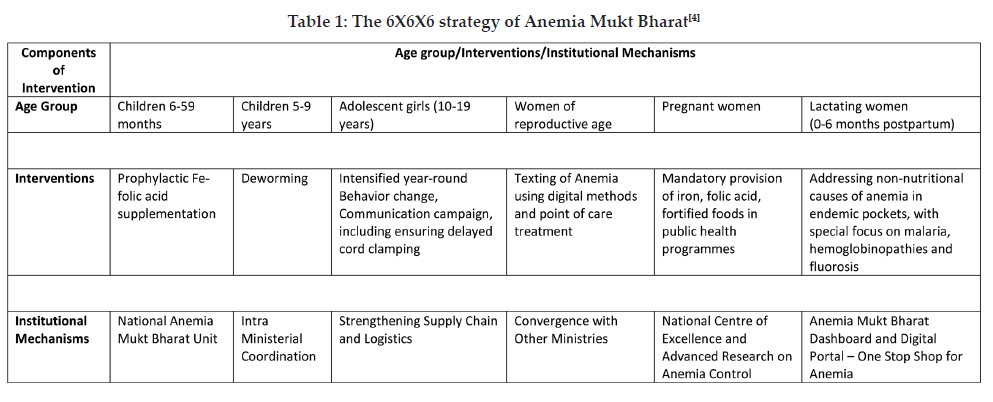
Anemia Mukt Bharat Programme
This program evolved from the Government of India’s National Nutritional Anemia Prophylaxis Program (NNAPP) in 2018. It is implemented by the Government with UNICEF. This is a 6X6X6 intervention along with Training Tool kits and Assessment (Anemia Mukta Bharat Index or AMB) of coverage of the target population with IS (Table 1). AMB program plans to reduce the prevalence of anemia by 2022. Unfortunately, the AMB index is based only on the doses of iron supplements delivered to the population and does not take into account how many cases discontinued IS due to side effects, and follow up hemoglobin measurements that are the factual indicators of the efficacy of the program.[4]
Anemia of Chronic Disease
This is of multifactorial origin and in order to diagnose this, it is important to determine the presence of chronic inflammation[5] viz infection, autoimmune disease, kidney disease, or cancer. Some physiological or pathophysiological problems that are associated with acute or chronic blood losses are also common causes of anemia. Bleeding in the gastrointestinal tract due to ulcers, growths and varices can also lead to anemia.
Chronic Anemia in Women
During the reproductive years menstruation itself may be a cause of iron deficiency anemia as is seen in menorrhagia, metrorrhagia and poly-menorrhea.[6,7]
Since iron deficiency is a large contributor to anemia, the terms iron deficiency, iron deficiency anemia and anemia are often, but incorrectly, used interchangeably.
Acceptance of Poor Health Standards for Indian Population
In general practice, subnormal levels of hemoglobin are easily accepted and go untreated because patients don’t have acute symptoms. Often, after treatment of acute episodes like hemorrhoids, ulcers or accidental bleeding, or heavy periods in women, no follow up investigations are advised to see if hemoglobin levels are restored. This attitude needs to be changed if we wish to eliminate anemia. The guidelines issued by the World Health Organization (WHO) for cut-offs vary according to age as follows: <11 g/dL for 1–4 years; <11.5 g/dL for 5–11 years; <12 g/dL for 12–14 years; <13 g/dL for 15–19 years; <12 g/dL for adult males and females. Out of the several biomarkers of Iron metabolism, apart from hemoglobin, serum ferritin level is the marker recommended by the World Health Organization to assess iron status and diagnose IDA in screening programs, with a caution to note any inflammatory conditions. The lower cut off for serum ferritin is <12 μg/L for 1–4 years, and <15 μg/L for 5–19 years, and accordingly it can be treated. Referrals are indicated when necessary.[6,7,8,9]
 Consequences of Anemia
Consequences of Anemia
The devastating long-term consequences of anemia are growth retardation in infants, children and adolescents, impaired cognitive development, poor mental and motor performance, reduced resistance to infection, reduced work capacity resulting in lower earnings, and an overall poor quality of life. Besides this, iron deficiency contributes to maternal morbidity and mortality including the possibility of preterm delivery with its hazards.
Heavy Metals in Relation to Anemia
Divalent metals like lead, cadmium, mercury and arsenic are taken up from the environment and may cause impaired cognitive development and irreversible physical and mental disabilities in association with anemia.[10]
Common Symptoms & Signs
Even mild symptoms like fatigue, weakness, pallor, dizziness, slight breathlessness on exertion, cold hands and feet, fast or irregular heartbeat, brittle nails, headache, difficulty in concentration, tiredness, leg cramps, can cause reduced work, exercise intolerance and minor dysfunction in the brain. The WHO has recognized this as the most difficult health problem leading to reduced productivity. Iron deficiency is the single most important nutritional risk factor in India, accounting for more than 3% of all disability-adjusted life years (DALYs) lost.[2] Usually patients seek treatment only when they have moderate or severe symptoms like pica and cravings for nonfood items, restless legs syndrome, sore tongue, shortness of breath, weakness, breathlessness on exertion, proclivity to infections, delayed response to treatment of infections. Severe anemia can lead to cardiovascular complications including edema on feet and cardiac decompensation.
Complications associated with IDA include heart failure, motor or cognitive development delays in children, pregnancy complications such as preterm delivery or having a low-birth-weight infant, depression, as well as high morbidity and mortality due to any other causes of illness.
Access to Health Services & Education
Difficult or absent access to health education and services, and non-affordability of treatment are all factors that leave many people, particularly women, untreated.
Limited Health Budget for Health expenditure as a proportion of Gross Domestic Product (GDP): The percentage of GDP allotted to health has been very low in India (< 1% in India vs 5% to 7% in some other Asian countries like Sri Lanka and Bangladesh, and about 10% in the USA). India was ranked 145th out of 180 countries on the quality and access of healthcare.[11,12]
Lack of Attention to Immune Consequences of Anemia
In general, there is a lack of concern that chronic anemia leads to increased incidence of infections and is associated with higher morbidity and mortality. Iron deficiency is frequently concomitant with chronic inflammatory disease; however, iron deficiency treatment tends to be overlooked.
Availability of a digital hemoglobinometer in every dispensary for all doctors, irrespective of the type of practice (Allopathy, Ayurveda, Homeopathy or Unani system), would help greatly in early and rapid detection and follow up of cases. Point of care tests should be available and will facilitate early detection, follow up and management of anemia.
Insufficient Knowledge About Iron Metabolism and Biomarkers for
Assessment of Iron Status
All cases of anemia are not meant to be understood and treated by hematologists. All general practitioners, consultants and paramedicals and nutritionists have to be made aware of the advances which have occurred in nutritional science, clinical nutrition and biomarkers for nutrition and anemia, and advances in treatment which have occurred in recent times. The methods of suspecting ‘Iron Refractory Iron deficiency anemias’[13] and their referral systems have to become common knowledge at primary, secondary and tertiary health care levels, apart from teaching institutes, because these cases usually require parenteral iron therapy.
Complementary Health Systems
The role of alternative or complementary systems of medicine, particularly, Ayurveda has been underestimated in India in spite of the fact that a large proportion of population is being treated with Ayurvedic formulations, which have been manufactured through scientific pharmaceutical processes and are known and popular because they cause less side effects as compared to Allopathic medicine. In the last decade, an attempt has been made to standardize the formulations because this aspect was not paid much attention to earlier and resulted in ineffective medicines that were sold over the counter. All physicians should ensure follow up of cases and ensure that anemia is treated and prevented.
In Ayurveda, twenty types of anemia like – syndromes have been described with individualized treatment. The role of plant – based molecules or phytoconstituents which may reduce the toxicity/ side effects of IS needs to be experimentally evaluated in view of the several phytoactives present in Ayurvedic medicinal plants which are used for the preparation of Iron supplements.[14]
Anemia in Pregnancy
Special attention is given to anemia in pregnancy because it adversely affects both the maternal and fetal outcomes. Taking care of IS in pregnancy undoubtedly improves these outcomes. The Government of India, for long, has given attention to this and recently The Federation of Obstetric and Gynaecological Societies of India (FOGSI) has undertaken this as a mission. Due to logistic difficulties and the occurrence of side effects, a large number of pregnant women still go to term in the anemic condition. In order to overcome this, FOGSI has demonstrated that in addition to oral supplements, when advisable the liberal and one time administration of intravenous iron is extremely useful in reducing the degree of anemia and improves maternal and fetal outcome.[15] This is always carried out in approved centres with special facilities and under the care of specialists. Intramuscular formulations are also available. These are very useful in building up iron stores in the liver and other tissues. However, for majority of women oral supplements are available and preferred and parenteral iron is administered only when anemia is of a moderate or severe degree with little time to make up before full term.
We definitely need to spread awareness and train all health personnel with the tools of ‘Anemia Mukta Bharat’ for tackling this humongous problem!
Role of Iron supplements, Nutritional supplements and Biofortified Food
It cannot be denied that poor nutrition is one of the major causes of anemia. However, when we refer to poor nutrition, a diet is likely be deficient in other micronutrients also. It is also important to treat gastrointestinal disease so that the IS are absorbed effectively. Targeted interventions are also recommended for specific groups who are vulnerable e.g. infants, young children and pregnant women, as well as cases of Irritable Bowel Disease.
Supplements: Four different iron preparations are used frequently for oral supplementation: ferrous sulphate, ferric sulphate, ferrous gluconate, and ferrous fumarate. Higher doses are intended to immediately improve the status and treat the anemia. There is good evidence to show that intermittent iron supplementation is almost as effective as is daily iron supplementation.[16] To some extent, prescribing in this manner may help to reduce the discontinuation of treatment due to side effects.
Food fortification: This approach aims at providing better nutrition security through improved diets to the target population. Generally, the nutrient that is deficient in the diet, in this context iron, is added to either foods or beverages. Fortification can also be done at point of use e.g., use of micronutrient powders or sprinkles. Fortification will not demonstrate immediate impact but it is believed to be a sustainable and cost-effective approach.
An important concern is that if several foods are fortified there is a risk of intake of excessive amount of iron resulting in iron overload and its detrimental effects. A case in point is folic acid which can reduce the risk of neural tube defects (NTDs). In 53 countries, national programs mandated the fortification of foods with folic acid to reduce NTDs. Revival of the practice of using iron tavas for making chapati/dosa, or iron utensils or iron ingots in cooking has been studied, but again there is concern about the potential iron overload in susceptible individuals.[17]
Provision of biofortified foods: Micronutrient malnutrition is also called ‘hidden hunger’. This hidden hunger is seen in persons who apparently consume adequate amounts of food, but these foods may largely be the staple cereals and some pulses that have lower volumes of micronutrients. The International Food Policy Institute estimates that more than 2 billion persons suffer from hidden hunger. In this scenario biofortification of staple crops is an effective way of reaching the large number of poor families, particularly rural families and helping their diets to be better in nutritional quality.[18] Biofortification uses agronomic practices, conventional plant breeding, or modern biotechnology to improve the nutritional quality / to increase the nutrient levels in the crops. This is a sustainable and cost-effective strategy, implementable at the population level wherein entire families can be reached instead of targeting only the person(s) diagnosed with anemia. Several crops have been biofortified e.g., rice, beans, sweet potato, cassava and legumes with iron; wheat, rice, beans, sweet potato and maize with zinc; sweet potato, maize and cassava with provitamin A carotenoid; and sorghum and cassava with amino acids and proteins. The Government of India has already taken an important step in linking agriculture and nutrition with biofortification.
Improving dietary diversity and quality: This is a very important and sustainable strategy that can help improve nutritional status of populations. The idea is basically to improve food variety through nutrition education, provision of foods rich in micronutrients or those that improve bioavailability of nutrients including approaches such as kitchen gardens etc.
Nutrition education, counselling: These are very important from the perspective of preventing anemia and promotion of good health but efforts to improve dietary quality and to encourage behavior change may take a long time. [19]
Acknowledgements: KHS-MRC has received a research grant for an experimental study on anemia, from the Rajiv Gandhi Science & Technology Commission (RGSTC), Maharashtra State, to explore the feasibility of improving bioavailability and reducing the oxidative stress from Iron Supplements.
References:
1. International Institute of Population Sciences (IIPS) and ICF. 2017. National Family Health Survey (NFHS-4), 2015-16: India.
2. World Health Organization. The global prevalence of anemia in 2011. WHO, Geneva, 2015.
3. Ministry of Health and Family Welfare (MoHFW), Government of India, UNICEF, Population Council. Comprehensive National Nutrition Survey (CNNS) National Report. New Delhi. 2019.
4. Anemia Mukta Bharat- A program by Government of India. 2018. Available from: anemiamuktabharat.info.
5. Cappellini M, Comin-Colet J, Francisco A, Dignass A, Doehner W, Lam CS, Macdougall IC, Rogler G, Camaschella C, Kadir R, Kassebaum NJ. Iron deficiency across chronic inflammatory conditions: International expert opinion on definition, diagnosis, and management. Am J Hematol. 2017;92(10):1068–1078.
6. Sunuwar DR, Singh DR, Chaudhary NK, Pradhan PMS, Rai P, Tiwari K. Prevalence and factors associated with anemia among women of reproductive age in seven South and Southeast Asian countries: Evidence from nationally representative surveys. PLoS ONE. 2020;15(8):e0236449. https://doi.org/10.1371/journal.
7. Sachdev HS, Porwal A, Acharya R, Ashraf S, Ramesh S, Khan N, Kapil U, Kurpad AV, Sarna A. Haemoglobin thresholds to define anaemia in a national sample of healthy children and adolescents aged 1-19 years in India: a population-based study Lancet Glob Health. 2021;9(6):e822-31.
8. Addo OY, Yu EX, Williams AM, Young MF, Sharma AJ, Mei Z, Kassebaum NJ, Jefferds MED, Suchdev PS, Evaluation of hemoglobin cutoff levels to define anemia among healthy individuals. JAMA Network Open. 2021;4:e2119123. doi:10.1001/jamanetworkopen.2021.19123
9. Lynch S, Pfeiffer CM, Georgieff MK, Brittenham G, Fairweather-Tait S, Hurrell RF, McArdle HJ, Raiten DJ. Biomarkers of Nutrition for Development (BOND)-Iron Review. J Nutr. 2018 Jun 1;148(suppl_1):1001S-1067S. doi: 10.1093/jn/nxx036.
10. Charles CV. Iron deficiency anemia: A public health problem of global proportions. Public Health – methodology, environmental and systems. May 2012;109-130.
11. Sinha Dipa. Explained: Despite Govt Claims, India’s Health Budget Only Around 0.34% of GDP. The Wire. Available from: https://science.thewire.in/health/union-health-budget-nirmala-sitharaman-covid-19-pmasby-allocation-gdp-expert-analysis/
12. Collaborators GB. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet. 2016; 390:1211-1259.
13. De Falco L, Sanchez M, Silvestri L, Kannengiesser C, Muckenthaler MU, Iolascon A, Gouya L, Camaschella C, Beaumont C. Iron refractory iron deficiency anemia. Haematologica. 2013;98(6):845-853. doi:10.3324/haematol.2012.075515.
14. Udipi SA, Joshi JV, Singh G, Sawarkar S, Phadke A, Prabhu A, Rastogi N, Vaidya AB. Phytoactives as Chelators of Iron with Potential to Mitigate its Side Effects and Enhance Iron Absorption. (MS submitted for publication).
15. Federation of Obstetrics & Gynecology of India. FOGSI General Clinical Practice Recommendations. 2020. Available from: https://www.fogsi.org/wp-content/uploads/2017/07/gcpr-recommendation-ida.pdf
16. Pēna-Rosas JP, De-Regil LM, Malave HG, Flores-Urrutia MC, and Dowsell T. Intermittent oral iron supplementation during pregnancy. Cochrane Database Syst Rev. 2015;10:CD009997.
17. Alves C, Saleh A, Alaofè H. Iron-containing cookware for the reduction of iron deficiency anemia among children and females of reproductive age in low- and middle-income countries: A systematic review. PLoS One. Sep 2019;14(9):e0221094. doi: 10.1371/journal.pone.0221094. PMID: 31479458; PMCID: PMC6719866.
18. Hurrell RF. Iron Fortification Practices and implications for iron addition to salt. J Nutr. 2021;151:3S-14S.
19. Girard AW, Dzingina C, Akogun O, Mason JB, MacFarland DA. Public health interventions, barriers, and opportunities for improving maternal nutrition in Northeast Nigeria. Food & Nutrition Bulletin. 2012;33:S51-S70. https://doi.org/10.1177/15648265120332S104.
+