A new kind of smart bandage developed at Caltech may make the treatment of these wounds easier, more effective, and less expensive. These smart bandages were developed in the lab of Wei Gao, assistant professor of medical engineering, Heritage Medical Research Institute Investigator, and Ronald and JoAnne Willens Scholar.
“There are many different types of chronic wounds, especially in diabetic ulcers and burns that last a long time and cause huge issues for the patient,” Gao says. “There is a demand for technology that can facilitate recovery.”
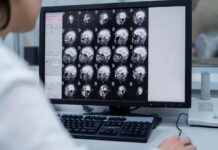
Unlike a typical bandage, which might only consist of layers of absorbent material, smart bandages are made from a flexible and stretchy polymer containing embedded electronics and medication. The electronics allow the sensor to monitor for molecules like uric acid or lactate and conditions like pH level or temperature in the wound that may be indicative of inflammation or bacterial infection.
The bandage can respond in one of three ways: First, it can transmit the gathered data from the wound wirelessly to a nearby computer, tablet, or smartphone for review by the patient or a medical professional. Second, it can deliver an antibiotic or other medication stored within the bandage directly to the wound site to treat the inflammation and infection. Third, it can apply a low-level electrical field to the wound to stimulate tissue growth resulting in faster healing.
In animal models under laboratory conditions, the smart bandages showed the ability to provide real-time updates about wound conditions and the animals’ metabolic states to researchers, as well as offer speed healing of chronically infected wounds similar to those found in humans.
Gao says the results are promising and adds that future research in collaboration with the Keck School of Medicine of USC will focus on improving the bandage technology and testing it on human patients, whose therapeutic needs may be different from those of lab animals.
“We have shown this proof of concept in small animal models, but down the road, we would like to increase the stability of the device but also to test it on larger chronic wounds because the wound parameters and microenvironment may vary from site to site,” he says.