Summary
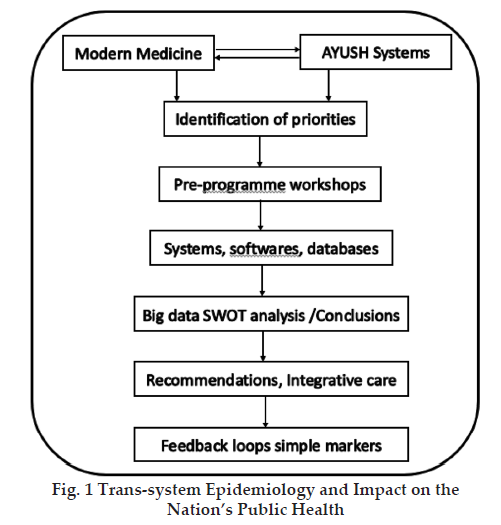
India has officially accepted pluralistic systems of medicine that include conventional medicine and the other AYUSH systems of medicine. Study of epidemiology and public health are often neglected in medical curricula of all the systems of medicine in India. It is essential to initiate endeavour for establishing trans-system epidemiology for health policy and its effective implementation. We present perspective for such an endeavour.
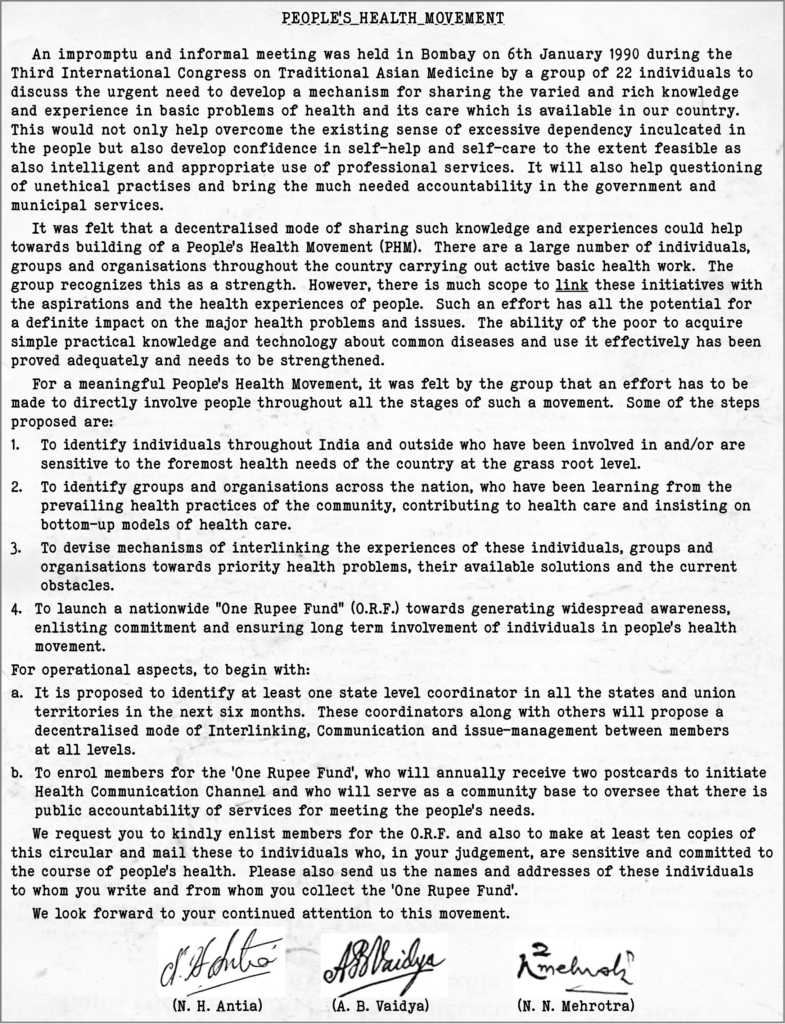
In an article, Dr. Devi Shetty, an eminent cardiac surgeon and Chairman and Founder of Narayana Health had stated, “WHO-ranking of Global Health Systems ranks India at a shameful 112th position, below Iraq and Venezuela, mainly due to the shortage of doctors.[1] His suggestions to improve this situation, are primarily focused on the Western bio-medicine and though valid, do not appreciate the pluralistic nature of healthcare in India which have gained more relevance in view of the proposal of “One Nation One Healthcare System” by the NITI Aayog of India.[2] Realizing the important role being played by the Indian Knowledge Systems of Health (currently termed as AYUSH), as long back as on 6th January 1990, during the “Third International Congress on Traditional Asian Medicine”, held in Mumbai, a group of 22 health system experts passed a resolution towards building a “People’s Health Movement” involving all these systems in Public Health.[3] This resolution was followed up later when one of the authors (ABV) was invited as an expert for National Commission on Macroeconomics and Health & Family Welfare, Government of India.[4]
Health Systems other than Western Biomedicine have been often termed as Complementary and Alternative Medicine (CAM), Traditional Medicine (TM), AYUSH (Ayurveda, Yoga & Naturopathy, Unani, Siddha, Sowa-Rigpa and Homeopathy) and Local Health Traditions (LHTs), besides Chiropractice, Osteopathy, Christian Science etc. The diversity of the basic principles and practice of these systems is daunting to even a polymath but the Covid-19 pandemic has made the world aware of both the glaring weaknesses as well as amazing strengths, unequally distributed among the systems.
However, for India one of the most common weaknesses amongst all these systems of health care has been the lack of organized public health and epidemiology which is required to meet the challenges of pandemics and the most common healthcare priorities of public health. The latter are often the most neglected subjects in medical pedagogy. Most of these Traditional Health systems which focus on personalized and individual patient care, hardly have these subjects in their syllabus. For a nation with pluralistic healthcare, it is most vital to have an agreement on diagnostic category; incidence and prevalence of diseases which pose major public health challenges and help make rational decisions for public health policy and its implementation.
Many years back we had proposed Ayurvedic Pharmacoepidemiology as a trans-discipline for integrative research and practice.[5] At that time competencies for big data analysis had not evolved. The paucity of essential software, raw data veracity, trained personnel and resources did not permit the nationwide application for a productive health data-base. However, a study was conducted in 2010 on ‘Status & Role of AYUSH & Local Health Traditions (LHT) under NRHM with startling epidemiological data on its wide coverage across the country, in order to help evolve a strategy for mainstreaming AYUSH & LHTs.[6] Recently, in a dialogue with the Secretary, Ministry of AYUSH, Government of India, the issue of big data analysis in AYUSH health care systems was discussed.[7] It is heartening to learn that the Government of India has already started big-data collection, and analysis at the national level, at least for Covid 19 management. What needs to be emphasized is to think out of the box, with a new vision of integrative epidemiology.
 It is imperative to have intersystem dialogues before a vision is proposed for a trans-system endeavour. Recently, the ICMR Product Development Centre (PDCs) at Kasturba Health Society’s Medical Research Centre KHS-MRC) in collaboration with ICMR’s National Institute of Research in Reproductive Health, (ICMR-NIRRH) are involved in developing India-specific guidelines for management of Polycystic Ovary Syndrome (PCOS). For the process of the development of guidelines, intersystem webinar-dialogues have been held between Modern Medicine and Ayurveda, Homeopathy and Siddha. That was indeed a learning experience underlining the urgent need for grass root substratum for a common trans-system epidemiology and public health measures. Similar initiatives are required for management of Covid 19 where AYUSH Guidelines have been prepared for its management.
It is imperative to have intersystem dialogues before a vision is proposed for a trans-system endeavour. Recently, the ICMR Product Development Centre (PDCs) at Kasturba Health Society’s Medical Research Centre KHS-MRC) in collaboration with ICMR’s National Institute of Research in Reproductive Health, (ICMR-NIRRH) are involved in developing India-specific guidelines for management of Polycystic Ovary Syndrome (PCOS). For the process of the development of guidelines, intersystem webinar-dialogues have been held between Modern Medicine and Ayurveda, Homeopathy and Siddha. That was indeed a learning experience underlining the urgent need for grass root substratum for a common trans-system epidemiology and public health measures. Similar initiatives are required for management of Covid 19 where AYUSH Guidelines have been prepared for its management.
In conclusion, the fact that The Indian Practitioner has taken the initiative of inviting experts to write on the major problems of public health, a series of thought–leadership articles, is a laudable step. Health being a state subject by the Indian constitution has always remained a challenge for key result areas in public health and TE. It is mandatory to make essential amendments in the constitution. But, to improve the ranking of our health care by WHO, we urgently need what can be best achieved for the major health issues, within the federal structure of our nation.
Acknowledgements
We thank Dr. P Manickam (ICMR-National Institute of Epidemiology, Chennai) and Research Director KHS-MRC, Dr. Shobha Udipi for their valuable inputs and Ms. Roda Dalal (Knowledge Cell- KHS-MRC) for editorial help in the preparation of this manuscript.
References
1. Shetty D. Transform Indian Health Care: How the government can build, at no cost, 300 new” Medical Colleges” and offer 30,000 new seats. The Times of India, Mumbai, June 14, 2019. https://timesofindia.indiatimes.com/blogs/toi-edit-page/transform-indian-healthcare-how-the-government-can-build-at-no-cost-300-new-medical-colleges-and-offer-30000-new-seats/
2. From HinduBusiness line Kochi | Updated on December 11, 2020 https://www.thehindubusinessline.com/news/centre-to-formulate-one-nation-one-health-system-policy-by-2030-minister/article33305905.ece
3. Antia NH, Vaidya AB, Mehrotra NN, The Indian Practitioner, 2021;Vol.74. No.9,33-35
4. Vaidya AB. Effective Integration of Indian Systems of Medicine in Health Care Delivery: People’s participation, Access and Choice in a Pluralistic Democracy. In NCMH Background papers, Financing and Delivery of Health Care Services in India. New Delhi: Government of India. 2005; 77-87.
5. Vaidya RA, Vaidya ADB, Patwardhan B, Tillu G, Rao Y. Ayurvedic Pharmacoepidemiology: A proposed New Discipline. JAPI.2003;51:528.
6. Shweta AS, Priya R. Status & Role of AYUSH and Local Health Traditions under the NRHM, NHSRC Study. 2010.
7. Kotecha R, Personal communication “The Intersystem Dialogue on India-specific Guidelines for Management of Polycystic Ovarian Syndrome (PCOS): Perspective of Siddha System of Medicine”.
Editor’s Note
There are several public health issues specific to India which need to be addressed comprehensively. The first task is to identify the serious public health issues and prioritize them in any plans of tackling them.
Broad based, well thought out initiatives are needed to manage these issues with well planned and well executed community health management strategies involving all stakeholders. These include from government health authorities to health care providers at all levels and of course patients.
These include government policy measures, creating robust healthcare infrastructure thru public-private partnership, adopting appropriate health care management approaches including new cost competitive and effective treatments, the use of technology from identification of such public health issues to consultation and health care delivery, creating proper awareness at all levels including in patients, upskilling of health care workers and establishing protocols for measuring patient outcomes.
For India’s teeming population due to the gargantuan health care challenges, relying only on the now widely used allopathic system is inadequate. We need to deploy other systems of medicine also, based on our traditional knowledge, but which need to be brought on par with western systems though scientifically approved evidence based research & clinical trials.
Call for Public health feature in The Indian Practitioner is started precisely to articulate the above mentioned issues, including the initiatives that need to be taken by different sectors of society, stakeholders and policy makers.
With this we are inviting doctors working on public/ community health issues to contribute articles for this feature. Email: theindianpractitioner@gmail.com
+


























